Advertisement
Grab your lab coat. Let's get started
Welcome!
Welcome!
Create an account below to get 6 C&EN articles per month, receive newsletters and more - all free.
It seems this is your first time logging in online. Please enter the following information to continue.
As an ACS member you automatically get access to this site. All we need is few more details to create your reading experience.
Not you? Sign in with a different account.
Not you? Sign in with a different account.
ERROR 1
ERROR 1
ERROR 2
ERROR 2
ERROR 2
ERROR 2
ERROR 2
Password and Confirm password must match.
If you have an ACS member number, please enter it here so we can link this account to your membership. (optional)
ERROR 2
ACS values your privacy. By submitting your information, you are gaining access to C&EN and subscribing to our weekly newsletter. We use the information you provide to make your reading experience better, and we will never sell your data to third party members.
Biological Chemistry
Preventing Malaria
Vaccine development already has taken decades, but recent clinical results show hints of progress
by Ann M. Thayer
October 24, 2005
| A version of this story appeared in
Volume 83, Issue 43

Malaria, a disease that afflicts hundreds of millions of people and causes more than a million deaths per year, can be prevented. The simplest way is to avoid the bite of a parasite-bearing mosquito, but this strategy is generally impossible in endemic countries where mosquito assaults are fierce. Spraying insecticides and treating bed nets can go far in controlling the mosquito vectors and reducing disease transmission, but vaccines are considered by many to be a long-term solution to prevent infection and disease.
Despite decades of work, researchers haven't yet created an effective malaria vaccine. Even if one were to exist, there would still be hurdles around purchasing and delivering it to the populations in need, as there are with other control and treatment measures. Scientifically, two challenges are key. One arises from the nature of the Plasmodium parasite itself-with its multistage life cycle and adaptability against attack. The other involves understanding and generating lasting, protective immune responses.
About 40 malaria vaccines are in clinical trials, according to data from the World Health Organization (WHO). Another 45 or so candidates are in preclinical development, along with about 20 at the research stage. They can be divided into four groups: preerythrocyte vaccines targeting the initial infection or liver stage of the disease; vaccines against the organism's blood stage, which is when symptoms appear; ones blocking parasite transmission to mosquitoes; and antidisease agents that reduce the effect of parasite toxins.
Several key organizations are helping to coordinate and support much of the research. These include the PATH Malaria Vaccine Initiative (MVI), European Malaria Vaccine Initiative (EMVI), National Institutes of Health, Wellcome Trust, and Special Program for Research & Training in Tropical Diseases (TDR). Most of the research takes place at academic, government, and private institutions.
Global funding for malaria vaccine R&D has totaled about $60 million to $70 million per year in recent years, says Melinda Moree, director of MVI, with NIH accounting for about half the total. MVI's budget has doubled in the past two years and this year will reach about $30 million; much of it comes from the Bill & Melinda Gates Foundation, which gave $50 million in 1999 to launch the initiative, followed by another $100 million in 2003. European Union and U.S. agencies, such as the Department of Defense and U.S. Agency for International Development (USAID), each spend several million dollars per year on malaria vaccine work.
Corporate involvement is limited, as many companies see few, if any, market-based incentives to invest in long-term, speculative, and expensive programs. Nevertheless, some firms, such as GlaxoSmithKline's vaccine unit GlaxoSmithKline Biologicals (GSKB), are making significant commitments to vaccine development. They and many small biotechnology companies have been encouraged by the support of public-private partnerships.
Companies are not here for charitable purposes, and we accept that, Moree says. So we try to find ways we can still work with industry. One approach taken by MVI is to give direct financial assistance. Another is to make the process more conducive to developing a vaccine, especially for small organizations, by establishing connections to clinical trial sites in Africa and pairing academic or government researchers with contract process developers and manufacturers.
Of the malaria vaccine candidates in development, roughly two-thirds are productlike, says MVI Scientific Director Filip Dubovsky, or based on technologies he believes might be scalable and economically feasible for making millions of doses. The problem in the past has been one of making well-characterized vaccines, as people had been taking shortcuts rather than a rigorous industrial approach, he adds. But that has really changed in the last five years.

Technological advances in making vaccines and a better understanding of the parasite have helped. For example, the parasite genome, unlike that of humans, yeast, or bacteria, is rich in adenine and thymine, a trait that necessitates changes on the genetic level in the organism used for recombinant vaccine production. Variable and complicated protein structure also is a factor because the parasite has learned to hide immunoreactive portions and avoid the human immune system.
Throughout its life cycle, the parasite presents different antigens at different times to the immune system. The sequencing of its genome in 2002 generated more than 5,000 potential targets and may eventually contribute to development efforts, but in the short term, having that many targets may not help. We still need to devote five to 10 years to turn antigens into proper vaccine candidates, Dubovsky says. And short of clinical trials, there's no screening tool that we know has a positive predictive value that something's going to work as a vaccine.
Robust animal models are lacking, he explains, and some vaccine candidates that appear to work in existing models fail to work in the field. People have been making vaccines against mouse malaria for decades, but that hasn't translated into [vaccines for humans], he says. In considering which candidates to support, MVI looks for demonstrated immunogenicity in a larger animal model along with good product characterization, stability, reproducibility, and a solid lab-scale process for manufacture.
Because we are at an empirical stage of development, we want to make sure any conclusions we draw from the data are absolutely spot on, Dubovsky says. That way we can either fail a product fast, or else we can push it forward into development.
The good news about malaria vaccine development, compared with other diseases, he explains, is that we can do challenge trials with preerythrocytic vaccine candidates, in which vaccinated individuals are exposed to the parasite and quickly show a response. Because the force of the infection is so incredibly strong, we can get an answer as to whether some vaccines have an impact in trials as small as 10 or 20 people. Even later stage efficacy trials may involve just several hundred people, which is a rare situation in vaccine development for infectious diseases.
A successful vaccine strategy requires an understanding of the human immune response. Unfortunately, the exact nature of this response isn't fully known for malaria. Humans develop a natural immunity to malaria after long-term exposure, although the immunity will wane when exposure stops. Immunity also is reduced in pregnant women. The onset of immunity depends on the intensity of malaria transmission, and the level of immunity largely impacts the severity of the disease. Most deaths occur among young children before they have developed protection.
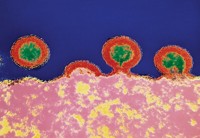
Researchers have been focusing on about 12 of 40 known antigens expressed during stages of the parasite life cycle. When an infected mosquito feeds on a human, it injects sporozoites into the bloodstream that quickly infect the liver. A so-called preerythrocytic vaccine targeting sporozoites would prevent all disease if it were 100% effective, but full-blown malaria could develop if even one sporozoite survived. Vaccines using blood-stage antigens mimic the natural immunity, so although still infected, a human host might suffer less severe disease. And transmission-blocking vaccines wouldn't help a patient but would prevent mosquitoes from spreading the disease. Many believe that the most effective vaccine will target antigens from more than one stage.
Results of a Phase IIb trial for the RTS,S vaccine have been called a breakthrough in showing that a vaccine might be possible. RTS,S consists of a recombinant polypeptide corresponding to part of the circumsporozoite protein (CSP) of Plasmodium falciparum, the parasite that causes the most deadly form of malaria, fused to a hepatitis B protein. The vaccine is believed to generate both antibody and T-cell responses to prevent the infection of liver cells and to destroy infected cells. GSKB developed the vaccine in collaboration with Walter Reed Army Institute of Research (WRAIR) over the past 20 years and, in 2001, entered into a partnership with MVI to accelerate development of the vaccine for pediatric populations.
In late 2004, GSKB and clinical collaborators reported that RTS,S with the adjuvant AS02A protected a significant percentage of children against clinical, including severe, malaria for at least six months (Lancet 2004, 364, 1411). In a test of 2,022 Mozambican children aged one to four years, the vaccine's efficacy was 45% against cases of infection and 30% against mild or non-life-threatening episodes of disease, and it reduced the number of cases of severe malaria by 58%. Follow-up results after 18 months will be available within a few months, GSKB researchers say.
Even such partial protection, many malaria researchers believe, is expected to have a substantial public health impact where the burden of malaria is very high. This prediction was borne out, MVI's Moree says, in a recent study sponsored by MVI and funded by USAID and the Gates Foundation. MVI is supporting another study at the Swiss Tropical Institute to predict the impact of a first-generation vaccine.
Other researchers, however, criticize what they deem a failure of RTS,S in creating sustained immunity for a sufficient length of time. In a recent opinion piece in Trends in Parasitology (2005, 21, 456), parasitologist Georges Snounou and colleagues in France question supporting onerous development programs that fall short of these goals, especially in light of proven affordable measures to alleviate suffering, such as insecticide-treated bed nets and combination [drug] therapies.
The RTS,S results are an important demonstration that a vaccine aimed at the initial stage of the infection has an impact on the clinical course of the disease caused by subsequent stages of the parasite life cycle, says Joe Cohen, GSKB's vice president for emerging diseases and HIV. A key to the recent success was 10 years of work on a formulation using the AS02A adjuvant to enhance an immune response, he adds. He is very hopeful that these enhanced immune responses will translate into sustained vaccine efficacy.
Remaining challenges include understanding the immunological mechanisms that underlie efficacy and demonstrating the vaccine's safety and efficacy in children under one year of age, Cohen says. A scalable manufacturing process is in place, and GSKB expects its RTS,S vaccine, Mosquirix, to enter Phase III trials in late 2007 or early 2008.
Recent results also have come out of Adrian V. S. Hill's lab at the University of Oxford. Hill uses antigens expressed in plasmid DNA or viral vectors to generate a T-cell-mediated immune response against liver-stage infection. The vaccine vectors encode for a construct that includes P. falciparum multiple-peptide epitopes and thrombospondin-related adhesion protein (Vaccine, published online Aug. 24, dx.doi.org/10.1016/j.vaccine.2005.08.048).
Using a two-stage prime-boost approach, Hill and collaborators found that priming immunizations with an attenuated recombinant fowlpox virus (FP9), followed by a recombinant modified vaccinia virus Ankara (MVA) vaccine, worked better than a DNA/MVA version in reducing infection (PloS Med. 2004, 1, e33). In subjects challenged with malaria, the FP9/MVA combination protected two of five subjects after six months and one after 20 months (Proc. Natl. Acad. Sci. USA 2005, 102, 4836). The Wellcome Trust, which supported the research, calls it the longest lasting protection yet seen.
Further studies in larger groups will take place with the FP9/MVA vaccine, the Trust says, with the real test to come in endemic areas. Following promising Phase I trials in Kenya, Wellcome researchers and collaborators have begun Phase IIb trials. Oxxon Therapeutics, a company founded by Hill and others that holds intellectual property rights to prime-boost technology, is involved as well. Hill's lab also has plans to collaborate with GSKB to test an MVA vaccine, expressing the CSP antigen, in combination with RTS,S/AS02A.
In June, Hill and colleagues were awarded a $10 million grant under the Gates Foundation Grand Challenges program (C&EN, July 4, page 9). Several of the 43 awards given will support malaria vaccine development programs, work on improved mouse models, and efforts to understand protective immunity.
Most malaria vaccine candidates have been designed around one or a few synthetic or recombinant antigen subunits. In addition to CSP, other subunit vaccines employ liver-stage antigens, such as LSA-3, that are believed to be associated with protective immunity. The most clinically advanced blood-stage vaccine targets merozoite surface protein 1 (MSP-1), thought to be involved in red blood cell invasion by the parasite. Blood-stage targets also include MSP-2 and MSP-3, erythrocyte-binding antigen-175 (EBA-175), and apical membrane antigen 1 (AMA-1).
Advertisement
WRAIR, GSKB, and MVI are working with the Kenya Medical Research Institute to conduct a Phase II trial of an MSP-1-based vaccine in children and are also expected to begin trials of an LSA-1 vaccine in 2006. Pasteur Institute will run Phase I/II trials of three LSA-3-based vaccine formulations. The institute recently completed a Phase I trial on an MSP-3 candidate with support from EMVI. In addition, NIH's National Institute of Allergy & Infectious Diseases' malaria vaccine development branch is conducting early-stage testing of an AMA-1 candidate and two MSP-1 vaccines, according to MVI.
On the basis of work by the International Center for Genetic Engineering & Biotechnology in New Delhi, India, Bharat Biotech International, in Hyderabad, India, is conducting human trials of a vaccine against P. vivax, the most widespread form of malaria. GenVec, meanwhile, is working with the U.S. Naval Medical Research Center (NMRC) to develop multistage, multiantigen vaccines using the company's adenovirus vector technology. NMRC is also working with USAID and Vical to develop plasmid DNA vaccines using one or more antigens.
There have been a number of notable disappointments. For many years, expectations were high for SPf66, a synthetic vaccine using antigens from two parasite stages, developed by scientists in Colombia. Early clinical trials seemed encouraging, but later Phase III trials demonstrated no efficacy. Likewise, the CSP-based ICC-1132 vaccine, developed by the now-defunct firm Apovia, recently failed to show protection (Vaccine 2005, 23, 857).
That most trials have concentrated on just a few antigens is a major concern, says Pierre Druilhe, director of the biomedical parasitology unit at Pasteur Institute, because there is already an extraordinarily huge amount of duplication that is a useless expense. He also believes that many antigens have been chosen inappropriately-for example, by looking for immunogenicity in mice. Plasmodium parasites are so specific and adapted to their hosts, he argues, that the only way to find a molecule that can be protective in humans is to look in protected humans.
Pasteur Institute scientists have sought to relate immune responses with resistance to infection through clinical observations. Studying the differences in responses among protected, unprotected, and infected subjects, and screening against potential antigens, allowed them to identify both MSP-3 and LSA-3. Results of the first MSP-3 vaccine trials showed long-lasting antibodies one year after immunization that were still effective at killing the parasite in vitro. Druilhe is encouraged by the results and says Phase II trials will determine if the vaccine-induced response will withstand challenge by the parasite.
Researchers are focusing on a subunit approach despite the fact that only one recombinant vaccine based on this approach-that against hepatitis B-is commercially available. Traditional vaccine development has focused on live, attenuated, or killed whole organisms. Nevertheless, the whole-organism route has long been considered impractical, if not impossible, for malaria vaccines, despite the decades-old finding that radiation-attenuated sporozoites offered more than 90% protection for at least 10 months.
One problem has been that attenuated sporozoites must be produced in mosquitoes and have been administered to humans only via direct exposure to more than 1,000 insects. We believe we can produce adequate quantities of these sporozoites practically and in a way that will meet regulatory guidelines, says Stephen L. Hoffman, chief executive and scientific officer at Sanaria. We also believe that a sporozoite vaccine can be delivered by a subcutaneous or intramuscular injection.
In 2002, Hoffman, former director of NMRC's Malaria Program, founded Sanaria, which now has support from several government agencies and the nonprofit Institute for OneWorld Health. The company is working to complete a manufacturing process and begin clinical trials in 2006. Although some skeptics have doubted whether Sanaria can actually produce such a vaccine, Hoffman says the irradiation process using controlled dosimetry to attenuate the sporozoites is precise and effective.
The sporozoites still are produced within the salivary glands of live mosquitoes, because no one has yet been able to reproducibly make highly infectious sporozoites in vitro, Hoffman says. After irradiation, the salivary glands are actually dissected from the mosquitoes by our staff and then the sporozoites are extracted, purified, vialed, and preserved. Although the eventual dose is yet to be determined, he expects that one mosquito could produce more than 100,000 sporozoites or about three to four doses of vaccine.
If the vaccine performs as anticipated, Hoffman believes it could prevent infection in 90% of individuals for at least a year, and possibly longer in endemic populations if natural exposure continues to boost protection. Our goal is to prevent severe disease and death in children, he says. But a vaccine with those characteristics would likely be attractive to markets in the developed world as well, including travelers and the military.
The vaccine we're developing has the potential to bring in enough revenue in the developed world to support its wide introduction at a deep discount in the developing world, Hoffman points out. This is the only way any vaccine has been introduced into the developing world.
Other researchers are producing genetically attenuated sporozoites (GASs) by knocking out specific genes. An attenuated sporozoite vaccine created by precise genetic manipulation will be safer, more reproducible, easier to produce, and possibly more potent than a radiation-attenuated sporozoite vaccine, says Stefan H. I. Kappe, a scientist at the Seattle Biomedical Research Institute.
Kappe and collaborators have shown that deleting single genes-either UIS3 or UIS4, which encode for sporozoite and liver-stage transmembrane proteins-arrested parasite development in the livers of mice (Nature 2005, 433, 164; Proc. Natl. Acad. Sci. USA 2005, 102, 3022). They also showed that immunization with knockout sporozoites resulted in complete protection against infectious sporozoite challenge. Researchers at Leiden University in the Netherlands, along with collaborators in Portugal and Germany, subsequently reported similar results after generating a GAS that lacks the surface protein gene P36p (Proc. Natl. Acad. Sci. USA 2005, 102, 12194).
The attenuation procedure by gene knockout is not very difficult, and the technology is available, Kappe explains. We plan to delete more than one gene, which will make it safer because the parasite is unlikely to find compensatory mechanisms that would allow it to grow. He is also optimistic that GAS production in mosquitoes can be scaled up. There is the option of producing sporozoites in insect cell cultures, he adds, although doing so will require a large effort and likely a consortium of companies, private donors, and research institutions.
The GAS work has used P. berghei, a species that infects rodents, but Kappe believes that the technology will translate directly to P. falciparum. Protection in the rodent model lasts for at least nine months, he says, which is the longest period between immunization and challenge they have tested so far. A five-year, $13.5 million Gates Grand Challenges Award will help the team advance the work into human malaria models and clinical testing at WRAIR.
Subunit vaccines based on individual proteins of the parasite have been tested, but they do not confer the desired high levels of protection. And most malaria researchers agree that a subunit vaccine is decades away, Kappe says. I think the Gates Foundation sees the opportunity to try an approach that can work in a relatively short period of time and that is substantiated by data.
Along with WRAIR, Kappe's collaborators include researchers at the University of Heidelberg, in Germany, and the Walter & Eliza Hall Institute of Medical Research (WEHI), in Australia. Louis Schofield, who heads the malaria immunology program at WEHI, is part of another international consortium with an $8 million Grand Challenges Award to develop ways to boost human immune responses. He is also working with chemistry professor Peter H. Seeberger at the Swiss Federal Institute of Technology (ETH), in Zurich, on a carbohydrate-based antitoxin malaria vaccine.
On the basis of Schofield's work uncovering the malarial toxin glycosyl phosphatidyl inositol (GPI) and Seeberger's chemistry expertise, they produced a synthetic GPI candidate and saw protective effects in mice (Nature 2002, 418, 785). Since then, Seeberger has refined the synthetic approach to a solution-phase process that can be more easily scaled up for making the target GPI hexasaccharide (Chem. Commun. 2004, 1706). Schofield, meanwhile, has been studying the mechanism of action of GPI toxins and testing vaccine candidates.
The basic principle of the antitoxin approach has been validated with a well-characterized synthetic molecule, Seeberger says. To help the human immune system respond to the hexasaccharide, the sugar will be linked to a carrier protein and combined with an adjuvant. Although this type of vaccine won't prevent infection, it may reduce the severity of disease and lower mortality. The technology has been transferred to Ancora Pharmaceuticals, a company cofounded by Seeberger and Schofield in 2003.
Ancora has been developing a manufacturing process to generate material for continued preclinical testing and eventually for clinical trials within three to four years, says John Pena, the firm's president. Polysaccharide-based vaccines typically use up to a few tens of micrograms of material per dose. Using a building-block approach, Ancora has been able to increase the synthetic yield and enable the production of kilograms of starting materials while significantly decreasing the overall cost of production.
Advertisement
The cost of new malaria vaccines remains a significant issue. GSKB admits its malaria vaccine is expected to cost more than other childhood vaccines being delivered through WHO's Expanded Program on Immunization, in part because it is being developed with the newest technology available. The volumes purchased by the public sector, whether contracts are guaranteed, and the duration of the contracts will also impact the price, the company says.
Most countries that would use these vaccines will be dependent on donor funding to purchase them, MVI's Moree says. Advanced market commitments, or purchase agreements, are believed to be a mechanism that will help pull companies into development programs. Many believe there will be a private vaccine market as well.
Encouraged by the RTS,S results, the U.K. government pledged to purchase the malaria vaccine if it becomes available as a gesture to help bolster a market, leverage additional donations, and encourage vaccine development. In September, the U.K., France, Italy, Spain, and Sweden increased their support of the Global Alliance for Vaccines & Immunization (GAVI) by launching the International Finance Facility for Immunization (IFFIm).
The new IFFIm commitment, combined with $750 million from the Gates Foundation, gives GAVI at least another $4 billion over 10 years. GAVI was created in 2000 through a previous $750 million Gates grant and has received financing from other private contributors and 10 governments. GAVI disburses funds for vaccine purchases around the world, and funding existing vaccine needs for all diseases is expected to take $8 billion to $10 billion over the next 10 years.
The Gates Foundation and Wellcome Trust sponsored a Malaria Vaccine Technology Roadmap initiative this summer. More than 180 experts representing 100 organizations from 30 countries met to develop a vision, strategic goals, and priorities for malaria vaccine development. The bottom-line goals, expressed in their draft report, are to have a vaccine on the market by 2015 that has greater than 50% efficacy against severe disease and lasts more than one year and to have one that is 80% effective against clinical disease and lasts longer than four years by 2025.
I don't think anybody believes a vaccine is going to be a magic bullet, MVI's Dubovsky says. It's going to be one tool in the global toolbox to help control malaria. First-generation vaccines aren't expected to replace bed nets and insecticide spraying or to displace the need for drug therapies, and research and investments in both preventive measures and treatments need to continue. But he and others believe that, with a system for providing childhood immunizations in place, vaccines are worthwhile as a cost-effective, long-term solution.
We are finally testing the concepts we came up with 20 years ago, Dubovsky says. A number of candidates are moving forward, and I think we are going to soon see a tremendous amount of clinical data and knowledge gained and which of these leads pan out.
MORE ON THIS STORY






Join the conversation
Contact the reporter
Submit a Letter to the Editor for publication
Engage with us on Twitter