Advertisement
Grab your lab coat. Let's get started
Welcome!
Welcome!
Create an account below to get 6 C&EN articles per month, receive newsletters and more - all free.
It seems this is your first time logging in online. Please enter the following information to continue.
As an ACS member you automatically get access to this site. All we need is few more details to create your reading experience.
Not you? Sign in with a different account.
Not you? Sign in with a different account.
ERROR 1
ERROR 1
ERROR 2
ERROR 2
ERROR 2
ERROR 2
ERROR 2
Password and Confirm password must match.
If you have an ACS member number, please enter it here so we can link this account to your membership. (optional)
ERROR 2
ACS values your privacy. By submitting your information, you are gaining access to C&EN and subscribing to our weekly newsletter. We use the information you provide to make your reading experience better, and we will never sell your data to third party members.
Biological Chemistry
Picking Apart Parkinson's
Researchers are seeking earlier detection and method to slow progression of disabling disease
by Sophie L. Rovner
April 10, 2006
| A version of this story appeared in
Volume 84, Issue 15

Investigators spoke with enthusiasm about advances in Parkinson's research during a recent conference, but the origins of the neurodegenerative disease and the means to stop it remain maddeningly elusive.
"Doctors and patients alike are growing frustrated with the current slow pace of bringing new therapies to market," said actor Michael J. Fox during the opening ceremony of the first World Parkinson Congress. Although funding hikes have increased research activity, they haven't yet unearthed a cure for the disease, let alone an effective long-term treatment for symptoms. "I did a search on PubMed, and there were 15,000 citations about Parkinson's over the last seven years," noted Fox, who was diagnosed with young-onset Parkinson's disease in 1991. "But I'm not tying my tie any faster."
Fox is more than a spokesman for the disease. His foundation is the largest nonprofit funder of Parkinson's research. The conference itself was sponsored by the Movement Disorder Society, the National Institutes of Health, the U.S. Army Medical Research Acquisition Activity, and several other organizations. The meeting drew more than 3,100 researchers, physicians, advocates, and patients to Washington, D.C., on Feb. 22-26.
Parkinson's disease is the second most common neurodegenerative disease after Alzheimer's. Parkinson's afflicts 1 million people in the U.S. It spawns a galaxy of symptoms that initially affect quality of life and later become incapacitating.
Development of a tremor in one arm is typically the first warning sign for those stricken with the illness. As the disease progresses, voluntary movement throughout the body decreases and becomes slower. The patient develops rigidity or muscle stiffness and may become bent in posture. Balance can also become a problem. Some patients experience "freezing," a sudden but temporary loss of the ability to move. As brain damage spreads, many patients develop debilitating fatigue, severe constipation, and a decline in the sense of smell. Sleep disorders, depression, apathy, sexual dysfunction, cognitive impairment, and dementia often occur as well.
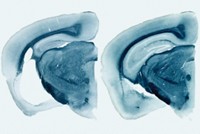
One of the main pathological hallmarks of Parkinson's disease is the deterioration and death of neurons that produce the neurotransmitter dopamine. Much of the neuronal damage occurs in the substantia nigra, a region in the midbrain that contains the cell bodies of the dopamine neurons. The axons of those neurons extend into the striatum, a section of the brain that controls movement. Loss of the dopamine nerve terminals in this region causes most of the motor symptoms of Parkinson's disease, said Stanley Fahn, chairman of the conference and director of the Center for Parkinson's Disease & Other Movement Disorders at Columbia University.
What causes the damage to dopamine neurons? The answer is multifaceted. "Rather than having one noxious factor, we are dealing with a plethora of factors," according to Serge Przedborski, a neuroscientist at Columbia. "I believe this cascade of multiple factors interacts to lead to the demise of dopamine neurons."
The details are sketchy, but the progression probably begins when a healthy dopamine neuron is exposed to an initiating factor such as abnormal α-synuclein protein, Przedborski said. He thinks the initial damage is exacerbated by secondary stressors such as protein aggregation, oxidative stress, mitochondrial dysfunction, hyperactivity in some parts of the brain due to the loss of dopamine, and activation of microglia. Microglia are central nervous system tissues made up of small cells that resemble macrophages.
The brain normally uses microglial cells to respond to an immune challenge, but microglia can also be activated by damage to neurons. In fact, microglia in Parkinson's patients become excessively active, giving rise to persistent inflammation in the brain. The cells secrete proteins such as interleukin-1β and inducible nitric oxide synthase. These cytotoxic molecules "flood the environment and stress neighboring compromised neurons, which are pushed to the edge and die, in turn activating more microglia," Przedborski said.
Dopamine neurons aren't the only ones to suffer damage. Parkinson's disease also kills neurons that produce norepinephrine and serotonin. Declining levels of these two neurotransmitters cause some of the mood changes and other nonmotor symptoms of Parkinson's, Fahn said. Death of neurons that produce the neurotransmitter acetylcholine leads to attention problems and dementia.
In addition to the destruction of neurons, the other major pathological feature of Parkinson's is the formation of Lewy bodies inside neurons. These protein deposits appear first in the lower brain stem. As the disease worsens, Lewy bodies begin appearing higher in the brain stem, then in the substantia nigra, and eventually in the cerebral cortex.
"Years ago, we used to think that Lewy bodies were the cause of the disease," Fahn said. "Now we think it may be the other way around."
"The Lewy body may not be about cell death or destruction at all, but it may be about protecting the brain," added David J. Brooks, a neurologist at Imperial College, London.
Several pieces of evidence back this idea. First, the order in which neuronal functions deteriorate doesn't correlate with the order in which Lewy bodies appear in the affected brain regions, Brooks said. Furthermore, at least one type of Parkinson's doesn't generate Lewy bodies. And Lewy bodies are found only in neurons that are still alive, Fahn noted. So it's possible, he suggested, that Lewy bodies "may be a protective mechanism to fight the degenerative process. Maybe they're tying up toxic proteins that otherwise would kill the neurons." Once the level of toxic proteins reaches a critical mass, the Lewy bodies are overwhelmed and release their toxic cargo, which kills the neurons, he hypothesized.
Lewy bodies consist primarily of filaments of misfolded α-synuclein protein polymers known as fibrils. The function of normal α-synuclein isn't known for sure, though Virginia M.-Y. Lee, a neurobiologist who heads the Center for Neurodegenerative Disease Research at the University of Pennsylvania, believes that the protein may play a role as a molecular chaperone in the formation of synaptic proteins known as SNAREs.
A number of factors promote buildup and aggregation of abnormal α-synuclein. For instance, the accumulation of oxidative stresses over a lifetime might promote phosphorylation of α-synuclein, creating an aggregation-prone form of the protein. And abnormal α-synuclein clogs the neuronal machinery that metabolizes normal α-synuclein and other proteins.
Just as the fundamental cause of the disease remains cloudy, researchers are also uncertain why one person gets Parkinson's but another does not. They have identified some factors that contribute to the risk of getting the disease, however. "Age is the most important risk factor for Parkinson's," Fahn noted. Most cases are diagnosed in patients who are at least 60 years old, though early-onset disease can strike people as early as their 20s.
Being male is another risk factor. At any given age, a man is 1.5 times as likely to get the disease as a woman. "Some people speculate that estrogen protects against Parkinson's," Fahn explained. Serious head trauma is also associated with increased risk for the disease.
Genetic mutations can cause the disease. To date, 10 mutations correlated with the disease have been identified in six genes, including the genes for the α-synuclein, parkin, and LRRK2 proteins.
The α-synuclein mutations enhance the protein's tendency to aggregate. The parkin mutations interfere with parkin's normal role in disposing of unwanted proteins. These unwanted proteins include misfolded versions of Pael-R, a receptor that is expressed on the surface of dopamine neurons and is thought to be involved in dopamine metabolism, said Ryosuke Takahashi, a neurologist at Kyoto University, in Japan. Accumulation of misfolded Pael-R and other toxic proteins, the thinking goes, adds to the stress that ultimately kills the neurons.
The mutations related to LRRK2, also known as dardarin, represent the most common cause of inherited Parkinson's that has been identified to date. According to Thomas Gasser, who led one of the teams that discovered the mutations, the mutations may alter LRRK2's participation in cell signaling, including its ability to phosphorylate yet unknown target proteins. Gasser heads the Hertie Institute for Clinical Brain Research at the University of Tübingen, in Germany.
Although mutations are involved in the disease, less than 10% of cases can currently be linked to inherited genetic defects. Most cases of Parkinson's are sporadic, meaning that they do not run in families. But at least some sporadic cases of Parkinson's are thought to be caused by mutations. If a mutation leads to disease only late in life, or if it increases the likelihood of getting the disease only slightly, "the family history may be obscured," Gasser explained.
Indeed, "there may be dozens of mutations yet to be discovered," according to Fahn. They might not have been recognized yet because they aren't sufficient in themselves to cause the disease. Instead, these mutations might interact with environmental factors to make one person more likely than another to get Parkinson's. For a person with such a "susceptibility gene," exposure to a particular environmental toxin could cause more damage to substantia nigra neurons than it could in someone without the mutation, Fahn added. "If you don't have the susceptibility gene, you might never get Parkinson's disease."
Environmental risk factors include rural living, drinking of well water, and exposure to metals in the workplace, said Yoshikuni Mizuno, a neurologist at Juntendo University School of Medicine, Tokyo. Pesticides and herbicides such as rotenone, paraquat, and diquat also appear to promote the disease, possibly by blocking the activity of mitochondrial complex I, the main component of the energy-processing machinery in a variety of cells, including neurons, said Caroline M. Tanner, director of clinical research at the Parkinson's Institute in Sunnyvale, Calif. Inhibition of complex I may increase mitochondrial production of reactive oxygen species that can harm the cells.
The multiple contributors to the development of Parkinson's offer plenty of opportunities to screen for the disease, including testing for mutations. Genetic testing might not be practical for the general population, at least until a cure for the disease is found. But it can be used to test family members of Parkinson's patients so they'll know whether they risk inheriting the disease.
Researchers are looking for other diagnostic tools to give early warning of the disease in people who don't have mutations. The ideal test would be able to diagnose the disease long before a patient realizes something is wrong. Why rush? Because by the time symptoms show up, the brain has lost at least half of its dopamine synapses. This devastating loss makes the goal of reversing the disease-assuming a treatment can be found-all the harder.
Alternatively, "we might be able to discover who is getting Parkinson's disease if we had a way to measure α-synuclein accumulation in the brain," Fahn said. A brain scan using positron emission tomography (PET) might reveal such deposits.
Neuroimaging is already being used to measure dopamine content in the brain, or at least to quantify functioning dopamine nerve terminals, Fahn said. A positron emitter such as [18F]-fluorodopa is taken up by dopamine neurons and stored in their nerve terminals. The terminals can then be detected with a PET brain scan.
Dopamine function can also be assessed with compounds that bind to transporter proteins in nerve terminals. Dopamine transporter proteins take up dopamine into the neuron after the neurotransmitter is released into the synaptic cleft. Vesicular monoamine transporter type 2 proteins store dopamine in vesicles in the nerve terminals. PET imaging compounds that can attach to these two types of transporter proteins include [123I]-2β-carbomethoxy-3β-(4-iodophenyl)tropane and [11C](±)-dihydrotetrabenazine.
Brooks noted that as the disease progresses, transporter binding declines and dopamine storage increases. "This is one of the adaptive mechanisms that help Parkinson's patients overcome the loss of dopamine in the brain," he explained. "If you're losing dopamine neurons, those that are left store more and transport less dopamine, so that it stays in the synapse and works on the receptors." The brain also boosts the number of dopamine receptors to compensate for the loss of dopamine, Brooks said.
Researchers are examining other ways to look for evidence of Parkinson's. For example, "screening the population for sense of smell may be one way of detecting early cases of Parkinson's disease before people develop motor symptoms," Brooks said. That's because the olfactory bulbs become atrophied in Parkinson's patients as a result of Lewy body pathology.
Advertisement
Parkinson's also damages nerves connected to the heart early in the course of the disease, Mizuno noted. This damage can be detected with a heart-scan technique known as scintigraphy using the imaging agent [123I]-m-iodobenzylguanidine.
Tests based on biological fluids are also in the works. Brigham & Women's Hospital neurologist Michael G. Schlossmacher and his team at Harvard Medical School have developed an enzyme-linked immunosorbent assay (ELISA) that can measure α-synuclein in blood, cerebrospinal fluid, and other biological samples.
In addition to identifying people at risk for Parkinson's or unambiguously confirming a diagnosis, researchers want to be able to use biomarkers to measure the impact of treatment. Such a test would be particularly useful in assessing the effectiveness of neuroprotective developmental treatments, which are desperately needed.
Several medications are available to treat the symptoms of Parkinson's, including the dopamine precursor levodopa (l-dopa), the most effective and widely used therapy. But the struggle to develop interventions to slow Parkinson's has been marked by failure, according to Karl Kieburtz, a neurologist at the University of Rochester. "Nothing slows the progression of Parkinson's disease, despite many studies and a lot of time invested," he said.
Furthermore, the available treatments "become less effective over time as the underlying disease progresses," Kieburtz said. For instance, L-dopa, which initially erases the symptoms of the disease, eventually leaves patients with several hours each day in which the medication is less effective. In addition, long-term treatment with L-dopa often causes its own sometimes debilitating side effect, an involuntary writhing motion known as dyskinesia.
Other available treatments include dopamine agonists such as pramipexole and ropinirole, which substitute for dopamine by activating dopamine receptors, Fahn said. Compounds such as entacapone and selegiline can be used to conserve dopamine by blocking the dopamine-metabolizing enzymes catechol-O-methyltransferase and monoamine oxidase B, respectively.
But compensating for the loss of dopamine "isn't the total answer to Parkinson's," Fahn noted. "Dopamine replacement doesn't reverse all the motor symptoms, and there are a lot of nonmotor symptoms that levodopa" doesn't fully address. These include depression, anxiety, passivity, dementia, sleep problems, and fatigue.
Because traditional tactics of drug development and testing have failed to turn up a satisfactory Parkinson's treatment, Kieburtz said, the National Institute of Neurological Disorders & Stroke (NINDS) is changing the rules of engagement. The agency's notion is to carry out quick clinical studies of promising compounds to see if they don't work. That way, he explained, "we'll avoid investing time and effort in things that are useless."
Kieburtz, a principal investigator for NINDS's trials of neuroprotective agents for Parkinson's disease, described a recent clinical trial involving 200 patients who were treated for a year with creatine, minocycline, or a placebo. By comparison, clinical trials to determine the effectiveness of a Parkinson's drug typically follow several hundred patients for at least two years.
The trial showed that creatine and minocycline are not, in fact, useless. Kieburtz warned that the results "do not equate to finding that the compounds are useful," but NINDS likely will study them more intensively in Phase III clinical trials.
The body-building supplement creatine was selected because it might counteract the mitochondrial dysfunction that develops in Parkinson's, particularly in neurons. The compound boosts energy production in cells, "which is likely to enhance their longevity," Kieburtz said. And minocycline is an approved antibiotic that has anti-inflammatory properties and may prevent cell death caused by microglial activation.
NINDS also tested coenzyme Q10, but the results of that trial haven't yet been published. On the basis of independent evidence, however, NINDS is seeking Food & Drug Administration approval for a Phase III clinical trial of CoQ10. This dietary supplement is a mitochondrial enzyme cofactor with antioxidant properties that might limit oxidative damage to neurons in Parkinson's patients.
Supplements aren't the only ordinary substances that may protect against Parkinson's. Incidence of the disease drops by about half in smokers, and not because smokers die at a younger age, noted Maryka Quik, a professor at the Parkinson's Institute. "We're focusing on the idea that nicotine may be involved," she said. "Nicotine interacts with nicotinic receptors in the striatum and substantia nigra. It stimulates dopamine release and alters locomotor activity." Studies also show that nicotine can protect neurons from damage by toxic compounds, including 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine (MPTP), which is used to create Parkinson's in animal models of the disease.
Coffee, tea, and nonsteroidal anti-inflammatory drugs appear to lower the risk for Parkinson's, Tanner said. Caffeine interacts with adenosine receptors, possibly triggering neuroprotective effects. NSAID pain killers may work by countering changes in the brain resulting from microglial activation and other inflammatory factors that contribute to the death of dopamine cells in the substantia nigra.
Parkinson's patients can also turn to an alternative to medication. Deep brain stimulation, which delivers electrical impulses to the brain with a pacemaker-type device, eases motor symptoms associated with the disease. DBS usually targets certain components of motor circuits in the brain that become overactive due to the loss of dopamine in Parkinson's patients, Fahn said. DBS quiets down these brain regions, shifting them back toward their normal state.
Andres M. Lozano, a neurosurgery professor at the University of Toronto who was one of the first to work on DBS, noted that studies are under way to determine whether placing DBS electrodes in other brain regions can help with the nonmotor symptoms of Parkinson's.
Researchers are also experimenting with biotech approaches to Parkinson's. For example, they are compensating for the loss of dopamine neurons by replacing them with neurons derived from fetal tissue or stem cells. Ole Isacson, a neurologist at Harvard Medical School, described a recent trial in which fetal neurons were implanted in the brain of Parkinson's patients. The transplanted neurons extended axons into a region of the brain where dopamine is normally released, allowing patients to stop their l-dopa treatments.
Jeffrey H. Kordower, a neurobiologist at Rush University Medical Center, Chicago, described the use of glial-cell-line-derived neurotrophic factor (GDNF). This brain protein enhances the production of dopamine and promotes the survival of dopamine neurons. Infusing GDNF into the brains of animal models of Parkinson's stops neuronal cell death. But the technique hasn't worked out in human clinical trials.
Researchers haven't given up on the growth factor, however. Kordower worked on a project in which the GDNF gene was transferred into human stem cells that were implanted in rats. The treatment improved motor symptoms.
Anders BjÖrklund, head of the neurobiology division at Lund University, in Sweden, is involved in a clinical trial in which semipermeable capsules containing epithelial cells engineered to produce GDNF are being implanted into patients' brains.
BjÖrklund is also testing a gene therapy approach in which a virus carrying the GDNF gene is injected into a patient's brain. The virus transfers the gene to the patient's neurons, which then begin making GDNF. The method has "given very promising results in both rodent and primate models of Parkinson's disease," according to Bjõrklund.
Ceregene, a company based in San Diego, is experimenting with a similar method to increase the brain's production of neurturin, a growth factor closely related to GDNF. Ceregene is sponsoring a clinical trial to test the safety of the approach. The researchers hope the additional neurturin, which increases expression of dopamine in the substantia nigra, will protect remaining healthy neurons and repair dying ones.
For now, researchers would be happy just to slow progression of the disease. But ultimately, Fahn said, "we'd like to cure the disease by reversing everything back to where it was before the patient developed Parkinson's."







Join the conversation
Contact the reporter
Submit a Letter to the Editor for publication
Engage with us on Twitter