Advertisement
Grab your lab coat. Let's get started
Welcome!
Welcome!
Create an account below to get 6 C&EN articles per month, receive newsletters and more - all free.
It seems this is your first time logging in online. Please enter the following information to continue.
As an ACS member you automatically get access to this site. All we need is few more details to create your reading experience.
Not you? Sign in with a different account.
Not you? Sign in with a different account.
ERROR 1
ERROR 1
ERROR 2
ERROR 2
ERROR 2
ERROR 2
ERROR 2
Password and Confirm password must match.
If you have an ACS member number, please enter it here so we can link this account to your membership. (optional)
ERROR 2
ACS values your privacy. By submitting your information, you are gaining access to C&EN and subscribing to our weekly newsletter. We use the information you provide to make your reading experience better, and we will never sell your data to third party members.
Synthesis
Drug Hybrids Enter the Fray
Combo molecules surpass components but sometimes work in unexpected ways
by Celia Henry Arnaud
November 12, 2007
| A version of this story appeared in
Volume 85, Issue 46

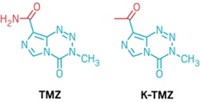
TWO DRUGS MAY BE BETTER than one, especially if they are parts of a single molecule. Hybrid drugs, just as their name implies, combine two drugs in a single molecule with the goal of creating a chemical entity more medically effective than its individual components. These combo drugs can indeed be more powerful than either of their precursors, and for reasons that aren't always what the drug developers expect.
Most tantalizing are hybrids that are much better than their respective building blocks. "Just by combining two molecules in the proper way, you sometimes have an activity increase of a factor of 100 or 1,000," says Michael Decker, a medicinal chemist at the Institute for Pharmacy at Friedrich Schiller University, Jena, in Germany. Although they are often combinations of approved drugs, no hybrid drugs, which from a regulatory perspective must be treated as new chemical entities, have themselves been approved as drugs.
A major driving force in the hybrid drug development community is to overcome one of the worst things that can happen to a drug: the development of resistance in its target population. In most such hybrids, the two druglike portions, also called pharmacophores, have independent modes of action that make the emergence of drug resistance less likely.
Chemist John J. Walsh, biologist Angus Bell, and coworkers at the Trinity College Dublin School of Pharmacy recently combined fast-acting artemisinin and slow-acting quinine into a hybrid drug for malaria, for which drug resistance is a barrier to effective treatment (Bioorg. Med. Chem. Lett. 2007, 17, 3599). Treatment with a fast-acting malaria drug by itself can lead to reoccurrence of the parasite Plasmodium falciparum, which causes the disease. But if in addition "you have a slow-acting antimalarial agent like quinine, there's a chance that it will kill the remaining parasites that haven't been killed by the fast-acting antimalarial agent," Walsh says.
Walsh and his coworkers connect the two drugs with a linker no more elaborate than an ester bond. "We were very careful to ensure that the activity of each molecule wasn't compromised by the site at which the two were linked together," Walsh says. Ester derivatives of artemisinin, such as the drug artesunate, don't adversely affect the parent drug's antimalarial activity, he notes.
In vitro assays show that the hybrid is more effective against drug-sensitive and drug-resistant malaria than the individual drugs alone or a cocktail made of a 1:1 molar ratio of the two. Walsh has several guesses about how the hybrid version improves the treatment's efficacy. The hybrid may increase cellular uptake, he says, noting that the lipophilic artemisinin can have problems getting into the cell's aqueous interior that the polar quinine can alleviate. "It's easy to make water-soluble salts of the combination," Walsh adds.
Artemisinin also shows up in the hybrid malaria treatments that the French company Palumed is developing. These so-called trioxaquines, first reported in 2000, combine artemisinin and chloroquine moieties in a single molecule (ChemBioChem 2000, 1, 281). Both drugs prevent the polymerization of heme into toxic hemozoin, but they act at different stages in the parasite's life cycle.
"The trioxaquine is able to alkylate heme like artemisinin does, while the quinoline entity is able to interact with free heme and block the polymerization," says Bernard Meunier, a pioneer of antimalarial hybrids and now chief executive officer of Palumed. The trioxaquines are the furthest advanced of the antimalarial hybrids. One of Palumed's compounds is in preclinical development at Sanofi-Aventis and is expected to enter clinical trials in early 2009, according to Meunier.
THE ANTIMALARIAL hybrid designed by David H. Peyton, a chemistry professor at Portland State University, in Oregon, combines the drug chloroquine with a so-called reversal agent, which counters resistance and is based on the antidepressant imipramine (J. Med. Chem. 2006, 49, 5623). The reversal agent inhibits a membrane channel that pumps chloroquine out of the parasite's digestive vacuole, the drug's site of action. The hope is that most of the hybrid molecules will continue to do what chloroquine alone usually does—bind heme and prevent the formation of hemozoin—and that the remaining hybrid molecules will take on the role of blocking the parasite's membrane pump.
The best of Peyton's hybrid drugs, called reversed chloroquines, are about 10 times more effective against drug-sensitive malaria than chloroquine by itself. Adding to this hybrid's promise is its ability to kill a chloroquine-resistant strain of P. falciparum.
Peyton believes that the hybrid has an advantage over a simple cocktail of the two drugs. In a cocktail, the reversal agent is unlikely to make it into red blood cells where the malaria parasites live, he says. In the hybrid, the reversal agent tags along with the chloroquine into the cells and then all of the way to the parasite's digestive vacuole. "If you do it as a cocktail, you need a much greater dose of the reversal agent" to get the same effect, he says.
Despite hybrids' promising properties and seeming advantages, a clear picture of how they achieve their effect is difficult to come by. The individual components may not have the same mode of action in the hybrid that they do as separate molecules. Even determining whether the two pieces remain connected in the living system is difficult.
The chemical bridge linking the two pharmacophores adds new dimensions to the drug developer's task. To keep the pharmacophores together, for example, the linker needs to withstand oxidation reactions in the cell that would otherwise sever the connection, Meunier says. "If you have fast oxidation or hydrolysis of the linker, then you get just the release of two drugs and it's more or less a prodrug approach."
THE LINKER itself can even end up exerting a greater effect on the activity of the combination than people assume or originally hoped. A recent example of a hybrid that combines aspirin and a nitric oxide donor is a case in point.
Aspirin is well-known to have many beneficial effects. Unfortunately, high doses can cause stomach problems. Because nitric oxide can block that toxicity, combining aspirin and NO in one molecule could provide the benefits of aspirin without its nasty side effects.
Postdoc Maikel Wijtmans of Free University, Amsterdam; undergraduate Niels Hulsman of Free University and the University of Amsterdam; and coworkers set out to figure out what gives one such aspirin-nitric oxide hybrid its antitumor properties. In this hybrid, the aspirin and nitrate are connected by a simple aromatic spacer.
The researchers lopped the pharmacophores off the hybrid one at a time, leaving the linker in each case. When they removed the aspirin moiety, the remaining portion of the hybrid was still very active. "Our curiosity was triggered," Wijtmans says. Something meant to be a simple three-month undergraduate project stretched out to 18 months. Eventually, he and his colleagues discovered to their surprise that the hybrid molecule's anticancer properties came from neither pharmacophore (J. Med. Chem. 2007, 50, 2424). "We chopped off both presumed pharmacophores and got a compound that was 10 times more active," Wijtmans says.
The nitrate part of the hybrid gets little chance to act as the nitric oxide donor it was designed to be. The hybrid is quickly hydrolyzed to aspirin and another fragment consisting of the spacer and the nitrate. This second fragment rapidly eliminates the nitrate to yield cytotoxic quinone methide. With this antitumor hybrid, the spacer turned out to be the active component.
"In the end, the function of the nitrate group was as a leaving group, while aspirin served only as a passive cap for the spacer," Wijtmans says. "The take-home message is that people should consider carefully what spacer they use" when designing hybrid drugs.
Perhaps that shouldn't be so surprising. After all, however familiar the building blocks may be, hybrid drug molecules are at their core new molecules, with identities independent of their precursors.




Join the conversation
Contact the reporter
Submit a Letter to the Editor for publication
Engage with us on Twitter