Advertisement
Grab your lab coat. Let's get started
Welcome!
Welcome!
Create an account below to get 6 C&EN articles per month, receive newsletters and more - all free.
It seems this is your first time logging in online. Please enter the following information to continue.
As an ACS member you automatically get access to this site. All we need is few more details to create your reading experience.
Not you? Sign in with a different account.
Not you? Sign in with a different account.
ERROR 1
ERROR 1
ERROR 2
ERROR 2
ERROR 2
ERROR 2
ERROR 2
Password and Confirm password must match.
If you have an ACS member number, please enter it here so we can link this account to your membership. (optional)
ERROR 2
ACS values your privacy. By submitting your information, you are gaining access to C&EN and subscribing to our weekly newsletter. We use the information you provide to make your reading experience better, and we will never sell your data to third party members.
Biological Chemistry
Resetting Priorities
The already challenging path to an HIV vaccine takes a hard turn after recent clinical trials
by Ann M. Thayer
September 22, 2008
| A version of this story appeared in
Volume 86, Issue 38

A HUSBAND AND WIFE have been infected with the same pathogenic strain of HIV for at least 10 years. While he must take potent antiretroviral drugs to suppress his infection and avoid its progression to AIDS, she requires no treatment because her body keeps the virus at undetectable levels.
"Elite controllers" or "long-term nonprogressors" such as the wife are rare, accounting for about one in 3,000 HIV-infected people, and the mechanisms keeping their infections in check are largely unknown, according to the Johns Hopkins University researchers who studied how her immune cells control the virus (J. Virol. 2008, 82, 7395). Any insight gained from such studies could be critical for the design of HIV vaccines.
Most HIV-infected individuals can't generate a durable response to control the retrovirus, which hijacks immune system cells in order to replicate and eventually destroys the body's disease-fighting defenses. The knowledge that elite controllers exist offers scientists some hope that an effective immune response via vaccine might be possible. Vaccines are widely considered to be the best means to curtail HIV's spread. In 2007, 2.7 million people became infected, and 33 million people lived with HIV, according to the Joint United Nations Program on HIV/AIDS.
Antiretroviral drug therapy has turned HIV into a largely manageable, chronic disease (see page 29) for the one-third of people who need the drugs and get them. It has helped slow the global HIV-related death rate to about 2 million per year. But treatment isn't a cure, and for every two people treated, another five become infected. Maintaining drug therapy indefinitely for all those who need it would be impractical and—at tens of billions of dollars per year—too costly.
"As good a job as we have begun to do in treatment, we still have a very important challenge in prevention," said Tadataka Yamada, Global Health Program head for the Bill & Melinda Gates Foundation, at the International AIDS Conference last month in Mexico City. Developing a vaccine "is still more of an art than science," he added. "Much of our vaccine portfolio that we work with today is based on empirical trials rather than on predictive, scientifically based trials."
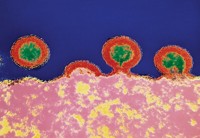
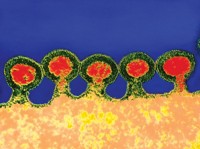
Work on an HIV vaccine began soon after the virus was identified 25 years ago. Unlike existing vaccines for polio, smallpox, and measles that use dead or live-attenuated (weakened) viruses to induce antibodies to block infection, an HIV vaccine using the whole HIV virus was deemed too risky. Instead, as they had done successfully for hepatitis B vaccines, researchers used just a viral surface protein against which the body makes antibodies.
In 2003, South San Francisco-based VaxGen reported results from the first large-scale human trials of an HIV vaccine. Based on a recombinant gp120 envelope protein, the company's AIDSVax, although safe, gave no protection.
Disappointed after VaxGen's trials, researchers quickly turned to different strategies. HIV can rapidly mutate and evade immune system attacks, an ability that renders antibodies ineffective counteragents. So rather than trying to generate antibodies, many researchers started trying to elicit cellular responses, knowing that the body calls on T cells to fight HIV. To do so, they devised ways to deliver viral subunits or genes to the body to cause an immune response against HIV proteins and antigens.
"The inner core proteins of HIV don't mutate as much as the envelope protein," explains Michael N. Robertson, Merck & Co.'s director for clinical research in vaccines and infectious diseases. Merck scientists launched a vaccine effort in the early 1990s and after much testing found that their best candidate vaccine was one containing three HIV genes for these core proteins in a recombinant adenovirus 5 vector. So-called Ad5 is one in a large family of common-cold-causing adenoviruses used as gene-delivery vehicles.
AFTER SEEING solid protection in preclinical tests, Merck moved its vaccine into Phase I human trials in late 1999 and early 2000. "We found that the Ad5 vector elicited the best cellular immune responses that were comparable to what we had seen in monkeys," Robertson says. The nonreplicating vector had a reasonable safety profile, and Merck had processes for manufacturing it on a large scale, he adds.
"With all of that information together—we had a vector that elicited the types of responses we and others felt could lead to an effective vaccine, it appeared to be generally well tolerated, and we could scale up—we thought that was enough to initiate an actual efficacy trial to see if this concept really worked," Robertson says.
"This was a novel concept," Robertson continues. "Even though other vaccines certainly elicited cellular responses, nobody had ever set out to design a vaccine that focused just on creating cellular immunity." Cell-mediated immunity wasn't expected to stop an infection from taking hold but possibly control the infection by reducing viral levels in affected people and thereby delay disease progression.
In late 2004, Merck and the HIV Vaccine Trials Network (HVTN), funded by the National Institute of Allergy & Infectious Diseases (NIAID), began the Phase IIb test-of-concept trial called STEP. After clinical researchers had enrolled 3,000 uninfected volunteers and waited 33 months, an outside board's interim analysis found no efficacy. In September 2007, vaccinations were stopped in the STEP trial and in another in South Africa that was using the vaccine. The outcome came as a blow not only to the trial organizers but also to the entire HIV vaccine field because Merck's vaccine had long been considered one of the most promising.
"The immune responses we got were very similar to what we got in our Phase I trials," Robertson says, but they failed to offer any protection. Subsequent analysis of the data indicated an even more alarming trend. "There were actually more HIV infections in people that got the vaccine than in people who got the placebo," he says.
"If we had not done this trial, people would still be spending millions of dollars and wasting years of time maybe pursuing a path that isn't ultimately going to get us a vaccine."
Because the vaccine contains virus fragments only, it cannot cause HIV infection. But people with prior exposure to Ad5, who had antibodies against the vector itself, appeared more susceptible to HIV infection. Overall, 82 people became infected. "If this was something that the vaccine caused, you would expect to see the effect more pronounced in people who had not been exposed to the vector before," Robertson explains, "because those are the people who seem to have the strongest response to the vaccine. But we saw the opposite of that."
This surprising and contradictory result is still being studied. Merck and HVTN are accepting proposals from outside investigators to analyze trial data and samples.
"Because we think this study is so important for the overall field, we have essentially opened this up to the outside world," Robertson says. "So far we haven't figured out why we saw an increased number of infections in a subgroup of people, and I don't know that we will."
Another question dogging HIV vaccine work is whether the Merck results signify the failure of one specific product or of the cell-mediated immunity concept overall. "I don't think anybody knows the answer to that right now, and for the past 15 years, the whole field has been focused on this T-cell vaccine approach," Robertson observes.
Fallout from the trial was behind the decision by NIAID Director Anthony S. Fauci to revamp and then cancel the Partnership for AIDS Vaccine Evaluation (PAVE) clinical trial. As originally designed, it was to be a Phase IIb proof-of-concept trial involving 8,500 people. It would have tested a two-stage vaccine developed by NIAID's Vaccine Research Center (VRC): a priming DNA plasmid delivering four HIV genes, followed by an Ad5 booster with three genes.
Although the VRC vaccine is believed to generate a more broadly functional T-cell response than Merck's, the booster's similarity meant it could be tested only in the least at-risk population—circumcised men without Ad5 antibodies. As a result, the PAVE trial was scaled back to 2,400 people. In July, Fauci decided, in agreement with some scientific leaders and contrary to the wishes of others, that the VRC vaccine didn't warrant a trial of this size at a cost of $65 million.
At the time, advocacy groups, such as the Treatment Action Group, in New York City, expressed concerns about vaccine trials and fear about the political, public, and scientific consequences if another large trial were to fail. The AIDS Vaccine Advocacy Coalition, although supportive, suggested that community input in the decision-making had been insufficient.
Even if the PAVE trial had shown promise, no one foresaw wide use of the VRC vaccine because of the prevalence of Ad5-positive people in the world. Still, Fauci's view is that the vaccine is scientifically intriguing and sufficiently different from other vaccines that NIAID will entertain proposals for a smaller, focused study with the specific goal of finding out whether the vaccine can lower viral levels in humans.
Despite the STEP trial's outcome, it still made valuable contributions in areas of trial design, execution, and results, according to Susan Buchbinder, a STEP cochair and HVTN investigator at the San Francisco Department of Public Health. "It was a pivotal trial for the vaccine field that brought us further forward than any single clinical trial to date," she told attendees at the conference in Mexico City.
"As good a job as we have begun to do in treatment, we still have a very important challenge in prevention."
SCIENTIFICALLY, the trial's impact was significant, not the least for being a reminder of how hard it is to create an HIV vaccine and highlighting the remaining challenges. It also incited intense discussion within the vaccine R&D community about the future of vaccine development and priorities for basic versus clinical research.
"It's a hard balancing act," Robertson says. "You can keep on playing around in the lab, but since we don't really have a perfect animal model for HIV, at some point you just have to do a human trial to really know if you are going down the right path.
"If we had not done this trial, people would still be spending millions of dollars and wasting years of time maybe pursuing a path that isn't ultimately going to get us a vaccine," Robertson continues. "We knew this wasn't going to be the end game, but knowing what we knew at the time, it was important to take that step. Now we have to be very circumspect and try to understand the findings before we move on."
HIV IS a unique and formidable pathogen, and researchers have made great strides in deciphering it and the human body's immune response to it, according to the International AIDS Vaccine Initiative (IAVI), a global public-private partnership founded in 1996 to develop preventive HIV vaccines. But there is still a lot left to learn.
Besides rapidly mutating to evade the immune system, HIV targets the very cells needed to fight infection. The retrovirus can infect humans by multiple routes and then quickly integrate its genetic material into their chromosomes. Only a brief window of opportunity is open in which to counter HIV before it creates a lifelong infection.
No one has ever been documented as recovering from HIV, IAVI points out. Because most people don't naturally fight off HIV, any vaccine must generate an immune response better than what the body can do on its own. Ideally, a vaccine would also work against the multiple, highly genetically variable strains of HIV that exist around the world.
But it's unclear what magnitude, breadth, or type of antibody or T-cell response is needed, much less how to make a vaccine that elicits it. Furthermore, the STEP trial has only highlighted the debate around the relevance and value of widely used assays, as well as animal models and surrogate viruses, for evaluating vaccines. And these, too, are critical areas targeted for further research and validation.
"Everybody has taken a giant step back to research, but we want to maintain a balance," says Carl W. Dieffenbach, director of NIAID's Division of AIDS, about how the major players in the field are weighing the emphasis on clinical versus basic research. Most of the $961 million spent worldwide on HIV vaccine R&D in 2007 came from public funding, and 84% of that was from U.S. sources. NIAID spent $497 million, of which 47% went toward HIV vaccine discovery and 38% to clinical research.
Advertisement
"We have to make sure clinical research is integrated into the discovery process," Dieffenbach explains. "It's a different mind-set, moving away from product development to research, where we are really focusing on asking and answering questions that will lead us to a vaccine." Although this shift is considered critical, there's a desire to redeploy, and not dismantle, a clinical research infrastructure that has taken years to construct, especially in developing countries.
Leaders in the field anticipate, however, that clinical trials will stay small to inform development, rather than become large ones aimed at product approval. "Until we have a hint of biological activity, I think they will remain these standard test-of-concept trials that are focused on a relatively small number where we can get an answer relatively quickly," Dieffenbach explains.
THIS SUMMER, NIAID announced its revised priorities for HIV vaccine research. In June, it created an HIV Vaccine Discovery Branch to help translate basic discoveries about HIV into advances in vaccine design and evaluation. "It's putting more people on the problem than in the past and giving it a focus and a home," Dieffenbach says.
The branch will have oversight of the Center for HIV/AIDS Vaccine Immunology (CHAVI), a consortium of university and academic medical center researchers. NIAID helped set up the consortium at Duke University in 2005 out of concern that none of the then-current vaccine candidates would succeed.
CHAVI is one of two projects under the Global HIV Vaccine Enterprise, an international alliance of organizations dedicated to accelerating the development of a preventive HIV vaccine. The alliance's other project is the Collaboration for AIDS Vaccine Discovery, funded in 2006 by $327 million in Gates Foundation and other grants over five years. It consists of 13 vaccine research consortia and five service facilities.
NIAID also is reconsidering the number and types of grants it awards in HIV vaccine development and is working to expand nonhuman primate research. "We need new ideas, better ideas, innovation, and new approaches," Dieffenbach says. The amount of money awarded "will depend upon the quality and merit of the applications," he adds.
Among NIAID's new initiatives are ones supporting investigators in basic vaccine discovery—it will award up to $10 million in fiscal 2009—and in highly innovative tactics to interrupt transmission (HIT-IT) of the disease, totaling another $4.5 million. NIAID has launched a $15.6 million, five-year program to study antibody-producing B cells through a network of 10 research teams.
As researchers turn upstream to find the answers they need to fundamental questions about both HIV and the human responses to it, the already highly scrutinized field is facing even more pressure. The harshest criticism, such as that voiced in a March 23 Baltimore Sun opinion piece by leaders at the AIDS Healthcare Foundation, suggests that vaccine research should be ended and the money diverted to testing, prevention, and treatment. At the same time, precisely because proven prevention and treatment tools exist, along with the resources to use them, International AIDS Society leaders suggest there's time for vaccine researchers to reflect before moving ahead.
"Failure is the norm in product development, particularly for something as difficult as HIV," IAVI President Seth Berkley says. IAVI, along with HVTN and others, was part of the PAVE clinical trial network. In conjunction with its partners, IAVI has moved six vaccine candidates into clinical trials. Although disappointing, the recent setbacks were not really surprising, Berkley adds.
"But the media has treated this as if it was the end of vaccine efforts, we haven't learned anything, and there is no science moving forward—and that is all completely untrue," Berkley says. "There is an active and vibrant effort going on, and we have a path toward where we need to go." In Mexico City IAVI released its annual Blueprint report, which outlines the major challenges and milestones.
IAVI was already building its programs around the idea that Merck's candidate was not going to be a "proverbial home run," Berkley says. Six years ago, IAVI started the Neutralizing Antibody Consortium (NAC) to foster collaboration on unearthing broadly effective antibodies that can block HIV infection. IAVI is expanding its effort, which complements others under way.
"We have a new focus on the problem and a diversity of approaches that is very healthy," Berkley says. "There is evidence in humans that it is solvable because humans do make the right types of neutralizing antibodies." Experiments have shown that these antibodies can protect monkeys from infection.
But most human antibodies don't pack enough punch, and the difficulty has been finding immunogens that can induce potent antibodies that can work against many HIV strains. VaxGen's vaccine, for example, did elicit antibodies, but they didn't neutralize nonlab strains of HIV. "The reason we focused so much on cellular immunity was that we didn't know how to generate broadly neutralizing antibodies," Berkley says.
In addition, HIV shields its surface proteins and binding sites from antibody attack. NAC has been able to characterize four neutralizing antibodies so far and has more targets at hand. "One antibody, 4E10, neutralizes virtually all strains of HIV," Berkley says. "But it is not an incredibly potent antibody, and the question is, 'Can you make these antibodies more potent?' "
Meanwhile, IAVI's Vector Design Consortium is looking at replicating vectors with HIV gene inserts to induce more potent and durable responses. Vaccinating monkeys with live-attenuated simian immunodeficiency virus (SIV), which can replicate only once, doesn't diminish SIV's ability to induce protection, but weakening it more makes the vaccine safer but less effective. "This suggests that replication is an important component to protection," Berkley says. Because the approach presents risks, IAVI has set up its own development labs.
RECENT EVENTS may bring other changes to the course and rate of vaccine development. Public-private partnerships such as IAVI often concentrate on managing a product development portfolio. Although IAVI and other developers together have had more than two dozen HIV vaccine candidates in the earliest stage of clinical testing, just a handful have advanced. IAVI also works with a wide network of partners in developing countries.
"IAVI will continue to have its clinical trial sites and capabilities for project management," Berkley says. "We have moved upstream a little bit more, but the value proposition is that as soon as there is interest and a product shows some promise, it can be rapidly moved into humans." About 90% of IAVI's support comes from public-sector grants, and in 2007, it spent $87 million, 71% of which went to R&D.
Given the difficulty of the science and limited business incentives, HIV vaccine research has never been very popular in the pharmaceutical industry. "Another fallout of the Merck trial is that whatever company interest was there has waned even further," Berkley says. "So we are even more dependent on the public-private partnership mechanism and public funding."
Several, mostly small biotechnology firms are among IAVI's scientific partners. To involve companies not working on HIV research but that might have applicable technologies, IAVI set up a $10 million innovation fund in 2007 with the intent of funding 15–20 small firms over three years.
In the future, as risks diminish in discovery and greater promise emerges in development, Berkley believes more big pharma companies will come into the HIV vaccine field. Besides Merck, large firms that have been involved include Sanofi Pasteur, Wyeth, and GlaxoSmithKline.
Merck is focused now on understanding the STEP trial results while maintaining its HIV research efforts. "Our plan was that this was going to work, and we were going to have a global HIV vaccine," Merck's Robertson explains. "We had put a lot of effort and resources into gearing up for the success of this vaccine, and with these results we felt that we needed to pause and try to figure out where we would go from here."
IAVI has recommended trimming and improving vaccine pipelines, diversifying away from cellular immunity, and including candidates that target neutralizing antibodies and immunity in mucosal surfaces across which initial infection occurs. "A new bar has been set," Berkley says. "I think you are going to see people moving away from the existing candidates or looking for ways to enhance them."
Some Ad5-based vaccine trials have been impacted because of concerns around using the vector. Although wide use of the Ad5 vector is extremely unlikely, NIAID's Dieffenbach says it is too early to determine whether the STEP trial results will knock out all candidates using adenovirus vectors, which had always been considered a good vaccine delivery platform. "We have to take each vector for its strengths and potential weaknesses and then make decisions on a vector-by-vector basis," he says.
EXACTLY WHAT kind of vaccine will be needed is also not yet known. "Some people believe a T-cell vaccine will have some biological activity and a public health benefit," Dieffenbach explains, "whereas others believe the only vaccine worth having is one that also protects against infection." A combination may be important because researchers have seen that HIV can break through an antibody attack. They believe T cells could mop up any circulating virus and prevent disease progression.
Advertisement
Even an imperfect vaccine that lacks high efficacy or broad coverage could have a dramatic effect against HIV, scientific leaders argue. The most advanced candidate in the pipeline is Sanofi Pasteur's preventive canary pox-vectored vaccine as a prime followed by a booster of what was VaxGen's AIDSVax. South San Francisco-based Global Solutions for Infectious Diseases has rights to the former VaxGen product. According to Sanofi, an independent monitoring board found no safety concerns and recommended in July that the 16,000-person Phase III trial under way in Thailand continue to its completion next summer. The vaccine generates T-cell and antibody responses.
Atlanta-based GeoVax Labs has a preventive vaccine candidate that it hopes to move into a large Phase II trial later this year, President Robert McNally says. The vaccine expresses three major HIV proteins in both a DNA prime and a modified vaccinia Ankara (MVA) booster. In Phase I studies the vaccine has elicited both T-cell and antibody responses, McNally says.
HVTN, the company's partner, has "taken a bit more conservative view," McNally says about whether to move ahead with trials. As of February, GeoVax believed its vaccine was only the fifth ever selected to move into Phase II trials. The company supports its work in part through a $15 million National Institutes of Health grant awarded in late 2007 and $10 million recently raised from investors.
"We have been approached by other agencies about proceeding into a therapeutic trial," McNally says. Vaccines would be given to already-infected people to generate an immune response to fight HIV. The idea is to reduce the need for daily oral medications and thereby more efficiently provide treatment and improve compliance. In animal studies, McNally says, GeoVax' vaccine performed therapeutically well against the SIV virus.
Danish vaccine developer Bavarian Nordic has refocused its strategy to emphasize therapeutic HIV vaccines, Chief Scientific Officer Paul Chaplin says. In 2007, the company reported that its MVA vaccine encoding the HIV nef gene controlled viral replication in a Phase II trial. With the idea that one gene was good and more might be better, the company has begun a Phase I/II trial of an MVA-multiantigen vaccine that encodes eight of the nine HIV genes.
MVA vectors don't seem to present the same problems as adenovirus vectors, Chaplin says, and they can generate strong immune responses without replication. Developers don't want to use replicating vectors for therapeutic applications and risk adverse events in immunocompromised patients, he explains.
COMPARED WITH tests of a preventive vaccine, those for a therapeutic one will quickly show any effectiveness on HIV replication in infected people, Chaplin explains. Although Bavarian Nordic worked with HVTN on earlier candidates, it now is conducting trials on its own. It might look for support again for larger trials, Chaplin says. "But it is much easier to get funding after you've gotten proof of concept in the clinic," he adds.
Both GeoVax and Bavarian Nordic are eager to advance their candidates. "It's debatable how valuable the animal models truly are, since some people have had very promising animal data but very poor clinical data," Chaplin says. "Our concept is to generate a broad T-cell response, and the only way to find that is to get into the clinic. Then, if you do generate that, you have to take a leap of faith and do a larger Phase III trial to see if it is actually efficacious."
Leaders in the HIV field are calling for other leaps of faith and innovations. In Mexico City, Gates Foundation's Yamada described HIV-related projects being funded under the $100 million, five-year Gates Grand Challenges Explorations program started in late 2007. An extension of the Grand Challenges in Global Health initiative, this newer program targets smaller projects at an earlier stage.
Calling it "venture capital for new ideas," Yamada said the program awards $100,000 for a selected idea in the first year, $1 million over the next two years for ideas that show promise, and even higher levels beyond that for truly novel ideas. The Gates Foundation expects to make about 60 awards during each round; the first proposal period ended in May.
Ideas proposed in the HIV area included focusing on host antigens rather than on virus antigens, reducing immune responses rather than enhancing them, and promoting more mutations rather than fewer. "All these are really challenges to dogma, which can hopefully lead to really new ideas for HIV vaccines," Yamada added. Proposals are being accepted now for a second round.
ALONG WITH a diversity of approaches, the HIV vaccine field is exploring other ways to keep its momentum. "We need to think of new ways of attracting and retaining young people," says Alan Bernstein, executive director of the Global HIV Vaccine Enterprise. "A lot of people went into the field in the '80s, when the virus was first discovered, and a new generation needs to come on who are, by definition, young and very familiar with newer technologies that they can apply to vaccine development.
"We need to do more basic science, but we need to start applying all the latest tools in biomedical research and in neighboring fields, including chemistry," Bernstein continues. Major funders around the world are thinking about new programs and putting new resources on the table to stimulate more basic science. "I think you have to tailor the programs and the resources to what you want to accomplish, so first we need to have a good discussion about what actually needs to get done," he adds.
Bernstein contends that recent events have highlighted the need for the vaccine enterprise, which serves as "a convener, neutral broker, and catalyst but doesn't fund any research." Proposed in 2003 and incubated within the Gates Foundation, the enterprise drafted a strategic plan in 2005 and received $20 million in Gates funding in 2007. In late 2007, it named Bernstein, founding president of the Canadian Institutes of Health Research, as its first head.
"Developing and delivering an HIV vaccine," Bernstein says, "has to be a global effort, and that's where the enterprise uniquely comes in because we're charged with bringing together people from all over the world—whether they are funders, scientists, governments, advocates, or industry—to work together."
Vaccine development has always relied heavily on empiricism. And even when successful, it has more often than not taken several decades to create a vaccine after finding the cause of a disease. "This is going to be a long haul," Bernstein says. "There are no quick wins, and we should stop thinking and planning like there are."







Join the conversation
Contact the reporter
Submit a Letter to the Editor for publication
Engage with us on Twitter