Advertisement
Grab your lab coat. Let's get started
Welcome!
Welcome!
Create an account below to get 6 C&EN articles per month, receive newsletters and more - all free.
It seems this is your first time logging in online. Please enter the following information to continue.
As an ACS member you automatically get access to this site. All we need is few more details to create your reading experience.
Not you? Sign in with a different account.
Not you? Sign in with a different account.
ERROR 1
ERROR 1
ERROR 2
ERROR 2
ERROR 2
ERROR 2
ERROR 2
Password and Confirm password must match.
If you have an ACS member number, please enter it here so we can link this account to your membership. (optional)
ERROR 2
ACS values your privacy. By submitting your information, you are gaining access to C&EN and subscribing to our weekly newsletter. We use the information you provide to make your reading experience better, and we will never sell your data to third party members.
Analytical Chemistry
Brain Glucose, Drop By Drop
Microfluidic device reveals link between glucose and patient outcome in brain injury
by Celia Henry Arnaud
October 25, 2010
| A version of this story appeared in
Volume 88, Issue 43
More than 1 million people sustain head injuries each year in the U.S. alone. The primary damage to the brain is apparent within minutes, but it isn’t the only thing patients and their doctors have to worry about. Secondary brain injury can occur days after the initial trauma, even in patients who seem to be recovering. Physicians need better ways to monitor patients who are at risk for secondary brain injury, and microfluidic devices that allow them to monitor brain chemistry could provide that better way.
Some brain injury patients experience a phenomenon known as spreading depolarization waves, in which brain activity decreases. In these waves, a chemical tsunami radiates from the site of injury, causing a drop in the potential across the membrane of cells in its path. “As these waves spread, they depolarize every neuron and every astrocyte they come into contact with,” says Anthony J. Strong, an emeritus professor of neurosurgery at King’s College Hospital, in London. Before those cells will again be ready to transmit signals, they must be repolarized, which requires large amounts of glucose.
“Quite often, you get another depolarization wave coming in before the tissue glucose has had time to recover from its work on the last depolarization,” Strong says. “If you look at the time course of tissue glucose in the injured brain, it’s a sort of downward staircase. Eventually you end up with no glucose. If there’s no glucose, you cannot repolarize, and those nerve cells will die.”
Monitoring brain glucose can give physicians an early warning that a patient is taking a turn for the worse. In conventional commercial analyses, the glucose level might be measured hourly, but glucose levels can change dramatically in a fraction of that time.
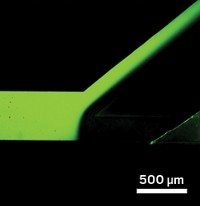
A droplet-based microfluidic method that is now being developed by Martyn G. Boutelle at Imperial College London will allow glucose levels to be monitored nearly continuously. Strong and Boutelle have teamed up to study use of the device as a monitor of brain glucose levels in brain injury patients. They are able to measure glucose on much shorter timescales than is possible with the periodic bulk sample collection methods used in the conventional commercial microdialysis approach.
In microdialysis, physicians implant a membrane-containing probe in a patient’s brain. They pump through the system an ionic solution, which elutes small molecules that have diffused across the membrane. They then analyze the components of the fluid. The problem is that the fluid must traverse more than a meter of tubing before being analyzed. At flow rates of 2 μL/minute, fluid can take as long as 15 minutes to get from the patient to the analyzer.
In a patient, Boutelle’s device works just like a conventional microdialysis probe, but Boutelle speeds up the measurement by converting the continuous flow into a segmented stream of aqueous droplets in oil, which cuts the time lag to seconds, he says.
“Segmentation of the sample stream preserves its temporal features when the probe outlet line is long,” says Adrian C. Michael, a chemistry professor at the University of Pittsburgh who has worked with conventional microdialysis. “Without segmentation, important temporal details can be lost due to diffusion as the sample travels along the outlet tubing.”
In fact, Boutelle is able to speed up the lag time from around 15 minutes to less than 15 seconds. With the droplets, the analysis is fast enough to acquire many samples and pinpoint when changes in glucose levels occur.
Boutelle measures the contents of the droplets with electrochemical sensors. At first, he put the electrodes directly in the droplet stream, but oil coated them and reduced their sensitivity. He and his coworkers solved this problem by putting the droplets back together when they reach the electrodes. This keeps the electrodes bathed in aqueous solution and prevents them from being fouled by oil. By carefully controlling the relative size of the droplets and analysis chamber, his team preserves all of the temporal information encoded in the droplets.
“As we have developed this technology,” Boutelle says, “we have gone from pooled samples of conventional microdialysis taken every 20 minutes to an hour to samples every 15 to 30 seconds using online flow-injection analysis to subsecond sampling with droplet-based microfluidics.”
“It’s showing us that the whole situation in brain injury is much more dynamic” than previously thought, Strong says.

So far, Strong and Boutelle are using the microdialysis-based glucose-detection device only with patients who need a craniotomy (surgery to open the skull) as part of their clinical management. The patients being so treated include those who have suffered trauma, a stroke, or an aneurysm. In those patients, a second device, a strip electrode, can simultaneously be placed on the surface of the brain to detect depolarization waves electrochemically.
Strong and Boutelle have used the strip electrodes to show that there is a relationship between the number of depolarization waves occurring and patient outcome. And depolarizations might not only be predictors of adverse outcomes; they might also help cause them, Strong says.
However, “we very much believe that these depolarization events occur in a lot of patients who aren’t sufficiently ill to need a craniotomy,” Strong says. “We’re working on the ability to do these same measurements in patients who don’t need that level of neurosurgery.”
If the group can show that electrochemical measurements of species such as potassium ions and glucose in the dialysate fluid accurately identify depolarization waves, using the strip electrodes could become unnecessary. Then microdialysis probes that monitor both glucose and depolarization could be implanted by methods somewhat less invasive than full-blown craniotomy, such as through small holes drilled in the skull.
A 16-center consortium called the Cooperative Study on Brain Injury Depolarizations (COSBID), founded by Strong and Boutelle among others, is investigating the role of brain depolarization in patient outcome. Jed A. Hartings of the University of Cincinnati, another founding member, is leading a five-center clinical trial within COSBID that will monitor as many as 180 patients with traumatic brain injury to determine whether depolarization waves observed while patients are in the hospital correlate with the patients’ neurologic status six months after their injuries.
One of the main hurdles, Hartings says, is determining cause-effect relationships between variables such as oxygen and glucose levels, blood flow, brain function, and depolarizations. Strong and Boutelle’s “technology will enable us to decipher those relationships,” he says. Once those cause-effect relationships are known, physicians will know which measurements will best help them treat patients.
Before it can be used more widely, the technology needs to be made more robust. “It’s a matter of making it user-friendly and as independent as possible from specialist scientific support,” Strong says. In the meantime, however, Strong and his colleagues regularly use the system. “We’re using this on every case we can,” he says.



Join the conversation
Contact the reporter
Submit a Letter to the Editor for publication
Engage with us on Twitter