Advertisement
Grab your lab coat. Let's get started
Welcome!
Welcome!
Create an account below to get 6 C&EN articles per month, receive newsletters and more - all free.
It seems this is your first time logging in online. Please enter the following information to continue.
As an ACS member you automatically get access to this site. All we need is few more details to create your reading experience.
Not you? Sign in with a different account.
Not you? Sign in with a different account.
ERROR 1
ERROR 1
ERROR 2
ERROR 2
ERROR 2
ERROR 2
ERROR 2
Password and Confirm password must match.
If you have an ACS member number, please enter it here so we can link this account to your membership. (optional)
ERROR 2
ACS values your privacy. By submitting your information, you are gaining access to C&EN and subscribing to our weekly newsletter. We use the information you provide to make your reading experience better, and we will never sell your data to third party members.
Business
High Hopes For Cystic Fibrosis
Two compounds to treat the underlying cause of the disease are nearing commercialization
by Lisa M. Jarvis
April 25, 2011
| A version of this story appeared in
Volume 89, Issue 17

More than 15 years of research and development is coming to fruition for the cystic fibrosis community: Two drug candidates that treat the underlying genetic defect causing the disease are on the verge of commercialization.
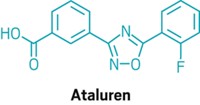
Vertex Pharmaceuticals expects to ask the Food & Drug Administration to approve VX770 later this year, and PTC Therapeutics should have a readout on late-stage trials for its drug Ataluren in early 2012. Although the drugs address just a small portion of the CF population, their success would be important first steps toward treating the underlying disease rather than just its symptoms.
CF is caused by a mutation in the CF transmembrane conductance regulator (CFTR) gene, which carries the instructions for assembling a protein that moves chloride ions from one side of epithelial cell membranes to the other. Some 800 different mutations in the CFTR gene have been documented, each causing a different malfunction. Most commonly, mutations result in a lack of protein at the cell surface to move chloride in and out; in other cases, the protein is abundant but not working properly.
As a consequence of the faulty protein, people with CF can’t maintain the right balance of hydration in their lungs, causing the organ to be dotted with dried pockets that become clogged with mucus. It’s a breeding ground for bacteria, and people with CF are saddled with a complicated regimen of medications to manage the chronic infections that the microbes cause.
Vertex’ VX770 addresses the 4–5% of people with CF whose disease is caused by the G551D mutation, which prevents the right flow of chloride ions in and out of cells. In February, Vertex unveiled data from a Phase III clinical trial suggesting the compound does indeed correct the genetic defect. At the end of the 48-week trial of 161 people with the G551D mutation, lung function improved by 16.9% in people taking VX770 compared with a placebo.
Surprisingly, younger patients—6 to 11 years old—appeared to respond better to the drug. “We were thinking we might have more difficulty detecting an effect, because their lung function was closer to normal,” says Chris Wright, medical director for the CF program at Vertex. “We think there may be more reversible disease in the younger patients, and this tells us that we should focus on getting treatment to patients as early as we can.”
Although unambiguous improvement in lung function is a key finding, Vertex scientists are also excited about some of the other improvements seen in the trial. The rate of pulmonary exacerbations—flare-ups that occur when the disease worsens, forcing CF patients to take other medications and antibiotics—dropped by 55% compared with a placebo.
By improving lung function and cutting pulmonary exacerbations, the drug could permit people with CF to take fewer medications overall. Vertex is still analyzing the data, and Wright says longer-term studies will be needed to understand whether any of the other drugs in the CF regimen can be eliminated or used less frequently.
Howard Liang, who follows Vertex stock for the investment firm Leerink Swann, says the data for VX770 far exceed expectations from industry watchers and could be “game changing” for people with CF. Vertex plans to file for approval of VX770 in the U.S. and Europe in the second half of this year.
Although the prospects for the first disease-modifying CF drug are encouraging, VX770 has only been effective in that small portion of the CF population with the G551D mutation.
Vertex has conducted in vitro studies that suggest the drug could also help people whose CF is caused by other mutations that, like G551D, hinder chloride ion flow. “We’re also doing some analyses of a variety of different mutations where we think we may have some positive effects,” Wright says. Vertex has yet to announce plans for clinical studies to test VX770 against those mutations.
Vertex did test VX770 in people whose CF is caused by the ΔF508 mutation, which results in not enough protein sitting on the cell surface, but the compound failed to improve lung function. Thanks to financial support from the Cystic Fibrosis Foundation, the company is pursuing two other compounds, VX809 and VX661, that both work to move more CFTR protein to the cell’s surface.
VX809 is already in Phase II trials. And earlier this month, the Cystic Fibrosis Foundation agreed to give Vertex up to $75 million over the next five years to support the development of VX661, which is expected to start Phase II trials by the end of this year. The compounds act by similar mechanisms to increase CFTR on the cell surface, and Vertex “hopes to make a decision between them” as data become available, Wright says.
Ultimately, the idea is to use VX809 or VX661 in combination with VX770 to maximize effectiveness in people with the ΔF508 mutation. Leerink’s Liang thinks the data validating the mechanism of action for VX770 mean a dual-therapy approach could work. He believes Vertex’ CF franchise could eventually be worth $500 million in annual sales.
A second firm’s drug to address a subset of the CF population is also nearing commercialization. PTC Therapeutics’ Ataluren is in a Phase III trial that is expected to be completed by the end of this year. Results should be unveiled in early 2012.
Ataluren addresses the roughly 10% of CF patients whose disease is caused by a “nonsense” mutation that prevents the full CFTR from being made. In normal cells, a ribosome attaches to the “start” site of messenger RNA and reads through the instructions for constructing the CFTR protein; with the mutation, the ribosome falls off early, rendering the protein inactive.
Ataluren enables the ribosome to continue reading through the protein recipe. In Phase II trials, PTC scraped cells from inside patients’ noses to test for the presence of the full protein and also to see whether it was actively moving chloride ions from one side of the cell to the other. The company showed that the full protein was being made, “which wasn’t seen in patients without the drug,” says Stuart W. Peltz, PTC’s chief executive officer.
The trials also demonstrated improvement in pulmonary function and a reduction in coughing in CF patients taking Ataluren. The Phase III study is testing the impact of the drug on people who have the nonsense mutation, who are six years of age or older, and who have some level of deterioration in lung function.
Peltz suspects few young patients are enrolled in the trial because of their better lung function. Yet in the long run, he says, children will ideally get the most benefit out of early intervention with the drug. “What you ultimately want is to have a kid who may have CF by genotype, but because of being on Ataluren never suffers from the physical characteristics that occur as a consequence of having CF,” he says.
The success of the Vertex and PTC compounds shows that the genetic defect that causes the disease can be fixed. And although the drugs work only in a subset of patients, researchers are encouraged by the progress in treating specific CF genotypes.
The field is on the cusp of “a new era where you have this genetics-based medicine that will go after the underlying cause of the disease,” Peltz says. “Now it’s a matter of finding other molecules for other mutations to help treat those patient populations.”



Join the conversation
Contact the reporter
Submit a Letter to the Editor for publication
Engage with us on Twitter