Advertisement
Grab your lab coat. Let's get started
Welcome!
Welcome!
Create an account below to get 6 C&EN articles per month, receive newsletters and more - all free.
It seems this is your first time logging in online. Please enter the following information to continue.
As an ACS member you automatically get access to this site. All we need is few more details to create your reading experience.
Not you? Sign in with a different account.
Not you? Sign in with a different account.
ERROR 1
ERROR 1
ERROR 2
ERROR 2
ERROR 2
ERROR 2
ERROR 2
Password and Confirm password must match.
If you have an ACS member number, please enter it here so we can link this account to your membership. (optional)
ERROR 2
ACS values your privacy. By submitting your information, you are gaining access to C&EN and subscribing to our weekly newsletter. We use the information you provide to make your reading experience better, and we will never sell your data to third party members.
Drug Discovery
Stapled Peptides Hit Puberty, With Attendant Drama
Dustup typifies challenges of a maturing field, say reinforced peptide experts
by Carmen Drahl
February 4, 2013
| A version of this story appeared in
Volume 91, Issue 5

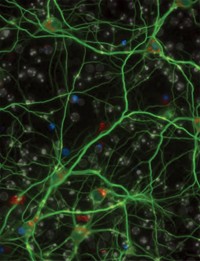
The concept of stapling means more than office drudgery to chemists these days. That’s thanks to stapled peptides, protein fragments chemically locked into an α-helical shape. They’re designed to be resistant to degradation, to penetrate cell membranes, and to bind tightly to disease target proteins.
Those properties have made stapled peptides valuable tools for probing disease pathways. They also make stapled peptides attractive as drugs: Boston-area researchers used them to launch a biotech company called Aileron Therapeutics, which on Jan. 14 announced plans for the first human clinical trial of a stapled peptide, to begin early this year. As with most “firsts” of this kind, many interested eyes are watching, from both a scientific-interest perspective and a business one.
But in December, a report by researchers in Australia and biotech company Genentech concluded that two stapled peptides didn’t perform as claimed (ACS Chem. Biol., DOI: 10.1021/cb3005403). To some chemists, the results could undermine Aileron’s efforts. The differing opinions aren’t surprising to experts, who say stapling technology is solid but that it can require laborious fine-tuning. The report is valuable, they say, because it raises important questions about reinforced proteins and drug development.
Many of the earliest peptides subjected to stapling were aimed at a family of cancer drug targets called Bcl-2 proteins. That’s how stapling caught the eye of Peter E. Czabotar, who studies Bcl-2 proteins at Australia’s Walter & Eliza Hall Institute of Medical Research. In the December report, Czabotar focused on two stapled peptides made from a portion of a Bcl-2 protein called Bim. What his team found, Czabotar says, runs counter to what researchers at Harvard Medical School and Boston’s Dana-Farber Cancer Institute published in 2008 (Nature, DOI: 10.1038/nature07396).
“The lesson as far as we can see is that the staple isn’t enhancing cell permeability or binding affinity,” Czabotar says. “Maybe there are other cases where the staple is an effective tool, but I can only comment on the peptides we’ve studied.”
Loren D. Walensky, of Dana-Farber Cancer Institute, led the 2008 research that the Australia/Genentech team scrutinized. He says his team never claimed that stapling alone guarantees cell permeability and enhanced binding affinity for any one peptide. Scientists might have to search through scads of different stapled peptides to find one with optimum biological activity, he adds. Walensky, one of the cofounders of Aileron, has published guidelines for designing effective stapled peptides, taking into account charge, hydrophobicity, and multiple factors including the staple itself (Curr. Protoc. Chem. Biol., DOI: 10.1002/9780470559277.ch110042).
“There’s not even a guarantee that stapling a peptide will stabilize a helix,” adds Gregory L. Verdine of Harvard University, Aileron’s other scientific cofounder and a onetime mentor of Walensky’s. In certain contexts, staples can stabilize nonhelical conformations, he says (J. Am. Chem. Soc., DOI: 10.1021/ja805037p).
Walensky says the new study’s conclusions are misleading because it uses a stapled Bim peptide that his group weakened on purpose for nuclear magnetic resonance work in 2008. Compared with his cell-permeable Bim peptide, the weakened peptide is more negatively charged and less helical in shape. These factors aid structural analyses but impair cell entry and biological activity, Walensky explains. The Australian team used the cell-permeable peptide in one experiment, but they used it on cells where Walensky’s team had shown they had no effect (J. Clin. Invest., DOI: 10.1172/jci46231). “The details matter here,” Walensky says.
Czabotar disagrees. He says Walensky’s team showed in 2008 that stapled Bim peptides could kill those particular cells, mouse embryonic fibroblasts. The results Walensky cites were published in 2012, when Czabotar’s team’s paper was still under review. “We went to great lengths to ensure we were using the correct peptides for the correct experiments,” Czabotar says.

To cancer researcher Sir David P. Lane, all of the scientists studying the Bim stapled peptide are top-notch. “And yet we’ve got a situation where their results are not consistent,” he says. “It’s a difficult situation to be in because this field has great promise.”
Lane speaks from experience. In the mid-2000s, Verdine’s lab sent him a stapled peptide designed to reactivate cell-cycle regulator and cancer drug target p53. In the Lane lab’s system, however, it didn’t work so well. With molecular modeling help from Chandra S. Verma, Lane designed next-generation molecules that “worked extremely well.”
“That’s about the time we started to hear rumors that others weren’t getting the stapling method to work,” recalls Lane, today chief scientist at Singapore’s A*STAR research agency. “Because we’d gotten positive results independently, that was puzzling.” He has since patented his stapled peptides and in December published further improvements to them (ACS Chem. Biol., DOI: 10.1021/cb3005148). With Verdine, Lane is planning a center in Singapore that will optimize certain stapled peptides for use in biochemical or animal tests. They will then make the peptides available for interested scientists to purchase.
David Cowburn of Albert Einstein College of Medicine and Asim K. Debnath of the New York Blood Center have gotten stapled peptides to work in cells. Their peptides interfere with HIV assembly (Retrovirology, DOI: 10.1186/1742-4690-8-28). “Stapling is not magic,” Cowburn says. He echoes Lane’s and Walensky’s accounts of the copious adjustments needed to obtain a peptide with solid activity.
Whether or not the Australian team used the appropriate stapled peptide for its studies, Cowburn says, it carried out a sound structural analysis to determine why its setup didn’t work. And because quite a bit of cutting-edge stapled peptide research is being conducted at companies, he adds, the lessons those firms have learned about making the most effective peptides aren’t necessarily available to everyone. “This is a case where a negative result was well worth publishing.”
At Tufts University, chemical biologist Joshua A. Kritzer thought the result was worth discussing with his students at group meetings. He told them not to look at the paper as a “he said, he said” situation, but as a call for chemists to take on the unknowns in the maturing constrained peptide field. “It’s not going to be sexy. It’s not going to cure anything,” he says. “But somebody has to do the grunt work to determine the factors that make stapled peptides and structures like them get inside cells.”
Not that Kritzer thinks nobody’s trying. In addition to the stapled peptide teams, he names R. Scott Lokey at the University of California, Santa Cruz, and Horst Kessler of the Technical University of Munich as leaders in pursuing the cell-penetration question. It’s a question, Kritzer says, that extends beyond stapled peptides to other peptides, natural products, and even macrocyclic drugs (ACS Chem. Biol., DOI: 10.1021/cb300515u).
A big challenge for stapled peptide drug development is how to measure levels of the peptides in tissues, Verdine notes. It’s relatively easy to measure levels of a molecule in the blood, and this is a reasonable surrogate for tissue levels with most small-molecule drugs. That’s not so for stapled peptides because they don’t equilibrate between the blood and the tissues in the same way, he says.
The Australia/Genentech work didn’t report anything new as far as the Aileron team is concerned, says the company’s chief scientific officer, Tomi K. Sawyer. He says several stapled peptides from academic labs have limitations from a drug development standpoint, such as weak target binding, insufficient activity in cells, or low efficacy in animals. That’s true of what he calls the “limited set” of Bim stapled peptides involved in the dustup. “We’ve made over 10,000 stapled peptides,” he says. “It’s hard work.”
In 2010, Roche paid Aileron $25 million—with the promise of up to $1 billion more in milestone payments—as part of a deal to jointly develop stapled peptide drugs. Last November, Aileron reported that a molecule developed within that partnership, ATSP-7041, triggered tumor cell death in animals through the p53 pathway. The first stapled peptide to be tested in humans will be ALRN-5281, which induces growth hormone. Aileron is developing that peptide independently. The company secured $12 million from venture capital firms to support Phase I clinical trials of ALRN-5281. Those trials will begin early this year, in patients with rare endocrine disorders. Aileron hasn’t disclosed structural details about either peptide.
Sawyer indicated that he hopes the Boston and Australia/Genentech teams will work out their scientific differences. “But that’s science for you. It isn’t always a gentleman’s game.”
“People assume science is linear, and it’s not,” Lane says. “There are personalities involved and opinions held, and it’s messy.
“We will work out the questions about stapled peptides in the future,” he says, “and it will be very exciting when we do.”



Join the conversation
Contact the reporter
Submit a Letter to the Editor for publication
Engage with us on Twitter