Advertisement
Grab your lab coat. Let's get started
Welcome!
Welcome!
Create an account below to get 6 C&EN articles per month, receive newsletters and more - all free.
It seems this is your first time logging in online. Please enter the following information to continue.
As an ACS member you automatically get access to this site. All we need is few more details to create your reading experience.
Not you? Sign in with a different account.
Not you? Sign in with a different account.
ERROR 1
ERROR 1
ERROR 2
ERROR 2
ERROR 2
ERROR 2
ERROR 2
Password and Confirm password must match.
If you have an ACS member number, please enter it here so we can link this account to your membership. (optional)
ERROR 2
ACS values your privacy. By submitting your information, you are gaining access to C&EN and subscribing to our weekly newsletter. We use the information you provide to make your reading experience better, and we will never sell your data to third party members.
Biological Chemistry
Polymer Nanoparticles Deliver Genes To Brain Tumor Cells
Nanomedicine: Genes carried by biodegradable polymer particles are efficiently expressed only in brain cancer cells in mice, but not in healthy brain cells
by Prachi Patel
May 8, 2014

Delivering genes that trigger cell death to tumors could be an effective way to fight glioblastoma, the most common and aggressive form of brain cancer. Now, researchers report biodegradable nanoparticles that can carry DNA into brain tumor cells in mice (ACS Nano 2014; DOI: 10.1021/nn501197v). The technique, which spares healthy cells, could be safer and more effective than other proposed gene therapy methods, the researchers say.
Currently, surgery is standard treatment for glioblastomas. Unfortunately, most patients survive only 15 months after treatment because their tumors usually grow back from cancerous cells that surgeons miss.
Scientists like Jordan J. Green, a biomedical engineer at Johns Hopkins University School of Medicine, think treating the sites of excised tumors with genes that promote cell suicide could improve patient survival. Doctors would inject materials loaded with DNA containing the genes during surgery. Any tumor cells remaining after surgery would engulf the materials, triggering DNA release and setting off their own death.
Hundreds of clinical trials have used modified viruses to deliver genes into cancer cells, Green says. But viral systems have significant downsides: They aren’t always effective, can be toxic in some primates, and can trigger an immune response in people. Other researchers are testing non-viral gene delivery vehicles such as liposomes, sugars, and polymers. These materials are decorated with molecules that target receptors found on cancer cells. But targeting isn’t always accurate, Green says. Healthy cells sometimes express the receptors, while some cancer cells in a tumor might not.
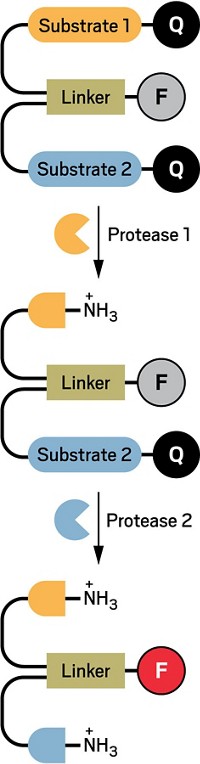
Green’s group previously designed a library of poly-β-amino esters with different side chains for gene delivery that do not target particular cell receptors. These polymers self-assemble with DNA to form nanoparticles that are nontoxic, degrade inside cells within a few hours, and can specifically deliver DNA to cancer cells in culture.
To demonstrate the method’s efficacy in live animals, Green and his colleagues, including neurosurgeon Alfredo Quiñones-Hinojosa, loaded nanoparticles with DNA carrying a gene for a red fluorescent protein. They injected these into tumors grown in the brains of mice. For comparison, they also injected the particles into the brains of healthy mice. After two days, they looked at cross-sections of the animals’ brains under a fluorescence microscope and saw that the volume of red-glowing tissue was six times greater in the tumors than in the healthy brain tissue.
Another experiment suggested that both cancerous and healthy cells take up the particles, but only tumor cells efficiently express the gene. The scientists injected nanoparticles tagged with red fluorescent dyes into the brains of healthy mice and animals with brain tumors. Unlike in the gene experiment, the healthy and cancerous tissues were equally red. The team is still trying to pinpoint the mechanism behind the difference in gene expression, but they think it might have to do with different ways tumor and healthy cells engulf the particles.
The work could be a milestone for treating malignant and non-malignant tumors, says Henry Brem, chief neurosurgeon at the Johns Hopkins Hospital, who was not involved in the work. “Being able to deliver DNA fragments specifically to brain tumor cells is breakthrough technology,” he says.




Join the conversation
Contact the reporter
Submit a Letter to the Editor for publication
Engage with us on Twitter