Advertisement
Grab your lab coat. Let's get started
Welcome!
Welcome!
Create an account below to get 6 C&EN articles per month, receive newsletters and more - all free.
It seems this is your first time logging in online. Please enter the following information to continue.
As an ACS member you automatically get access to this site. All we need is few more details to create your reading experience.
Not you? Sign in with a different account.
Not you? Sign in with a different account.
ERROR 1
ERROR 1
ERROR 2
ERROR 2
ERROR 2
ERROR 2
ERROR 2
Password and Confirm password must match.
If you have an ACS member number, please enter it here so we can link this account to your membership. (optional)
ERROR 2
ACS values your privacy. By submitting your information, you are gaining access to C&EN and subscribing to our weekly newsletter. We use the information you provide to make your reading experience better, and we will never sell your data to third party members.
Pharmaceuticals
What We’ve Learned From The Race For An Ebola Cure
Experts lament a thinner drug pipeline but point to promise in a new molecule from Gilead
by Lisa M. Jarvis
November 16, 2015
| A version of this story appeared in
Volume 93, Issue 45

Last year, at the height of the Ebola outbreak, Sina Bavari and Travis Warren found their labs at the U.S. Army Medical Research Institute of Infectious Diseases (USAMRIID) flooded with compounds for testing against the Ebola virus. Well-meaning drug companies hoping to help stem the crisis were offering anything that might have activity against Ebola to the government lab, which is one of only a handful of places in the country with a containment facility for screening molecules against the deadly virus.
Bavari and Warren were happy for the help but also overwhelmed as well as uncertain whether anything they were getting would actually work. Most of the compounds were developed for other diseases. Bavari, who is chief scientific officer of USAMRIID, compared the screening effort to trying to catch apples by holding a basket under a peach tree.
Fortunately, at least one apple seems to have fallen. In spring 2014, when the threat of the virus was starting to make headlines, Gilead Sciences shared part of its vast library of nucleosides and nucleotides with USAMRIID. Thus began a fast-moving collaboration that resulted in GS-5734, a nucleoside prodrug that has shown a remarkable ability to clear the virus in infected monkeys and is already being tested on healthy humans.
Gilead’s compound is a bright spot in a lean pipeline of Ebola drug candidates. Despite intensive work to find Ebola treatments and multiple clinical studies to evaluate their merit, scientists still aren’t sure which molecules are effective. They continue to press for answers while also preparing the world for the next epidemic—be it from the strain that caused last year’s outbreak or a different virus.
SCRAMBLING FOR A CURE
As cases of Ebola multiplied last year, government agencies, aid groups at the front lines of the epidemic, drug companies, and other stakeholders all worked together to determine how to design and roll out clinical trials for the handful of Ebola drugs that showed promise in infected monkeys.
Through that process, the infectious disease community learned that “we can accelerate the system,” says Daniel Bausch, a virologist at Tulane University and an Ebola expert. But setting up trials “has not been an easy process. It’s been kind of messy, and there has been mud wrestling and arguments and starts and stops.”
Much of the arguing was over how to design clinical trials. Purists such as the Food & Drug Administration wanted a traditional randomized controlled trial, meaning some patients get the standard of care plus an experimental drug and others just get the standard of care. Such trials are best at delivering clear answers about the efficacy of a treatment.
On the other end of the spectrum were advocates for single-arm trials, in which every patient receives the therapy. These trials might not provide a definitive sign that a drug works, but they at least allow drugs to be ruled out.
In the end, some studies were launched on a middle ground: They had an adaptive design that allowed investigators to get early peeks at the data and stop the study if a drug looked effective.
But by the time agreement was reached about clinical trial design, the epidemic had hit its peak and was starting to abate. That was good news for public health but bad news for evaluating available drug candidates. As studies finally started to roll out, there were fewer and fewer patients available to enroll in them.
“Getting things in place in the recent Ebola epidemic was quick compared to past experiences,” says Edward Cox, director of FDA’s office of antimicrobial products. “But it’s clear we need to think and plan to figure out ways to get trials in place even more quickly to be able to answer questions about which therapies are helping patients.”
Between the delays in starting trials, problems with trial design, and the usual setbacks encountered in clinical testing, experts are having a hard time pointing to a clear winner among the drugs that were assessed.
“If anything, treatment options have become more limited than they were last year,” USAMRIID’s Warren says. “We have some new things on the table, but some treatments that were previously used in patients were either shown to be ineffective or they’ve been discontinued.”
For example, Chimerix put its antiviral brincidofovir into an Ebola clinical trial in Liberia in December 2014, but a month later the company halted the test. Although Chimerix didn’t provide a clear reason for its decision, it noted the waning patient population.
Tekmira Pharmaceuticals, which has since been renamed Arbutus Biopharma, pulled the plug on a Phase II study of its RNAi-based drug TKM-Ebola-Guinea after an early analysis of the data suggested it wasn’t effective. Meanwhile, an RNAi drug developed by Sarepta Therapeutics that had shown some promise in monkeys never gained traction.
Only the antibody cocktail ZMapp—famously given to the first two American aid workers infected during the outbreak—and the antiviral favipiravir have demonstrated signs of working. The clinical trial of ZMapp continues, and Ebola experts believe it has at least some efficacy based on its use in foreign aid workers who contracted the virus.
Preliminary data from a study of favipiravir, from the Japanese firm Fujifilm, suggest the antiviral does not work for patients who have a high viral load but that it might help those with milder symptoms. Some researchers even question that result because the study lacked a control arm.
ZMapp isn’t a slam dunk either. Tulane’s Bausch points out that the trial had built-in checkpoints that allowed a data-monitoring board to look for early signs of efficacy. If the drug were obviously working—or obviously not working—the trial would be halted.
“The fact that you don’t have a result tells you two things: The results are not incredibly good nor incredibly bad,” Bausch says. ZMapp still holds promise, he adds, noting that the trial included patients who were probably beyond help, making clear signals of efficacy hard to see.
AN APPLE FALLS
The only new addition to the field is Gilead’s GS-5734, a nucleoside inhibitor that has done a great job of helping even the sickest of infected monkeys, according to Bavari. “If we wouldn’t have found the Gilead compound, I would probably still have nightmares like I did a year ago,” he says.

By conventional drug discovery standards, Gilead and its partners moved at breakneck speed to develop GS-5734. The process began as the crisis was ramping up in May 2014 and Gilead realized its deep experience with RNA viruses, a class that includes Ebola, might come in handy. After all, the company had a curative hepatitis C virus treatment on the market and a drug for respiratory syncytial virus in the clinic. Both are RNA viruses.
The big biotech firm shared selected compounds from its collection of roughly 9,000 nucleosides, or “nucs,” with both the Centers for Disease Control & Prevention and USAMRIID for screening. By the end of the summer of 2014, both labs came up with a handful of nucs with activity. Their efficacy “wasn’t spectacular, but they were certainly potent, and they looked better than other nucs that had been tried,” recalls Bill Lee, Gilead’s vice president of research.

The best lead out of the screen was a “c-nuc,” a nucleoside in which the sugar and base are connected by a carbon-carbon bond rather than a carbon-nitrogen bond. The base of the active molecule came from GS-6620, a c-nuc that had gone into Phase I studies as a hepatitis C treatment but was pulled owing to poor pharmacokinetic properties.
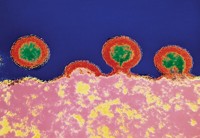
Gilead set out to make the compound better. Researchers believe the Ebola virus does most of its replication in macrophages, white blood cells that it uses as a breeding ground before striking epithelial tissue.
From its work in HIV, Gilead knew it could control where it delivered nucleosides and nucleotides. In fact, its antiviral tenofovir alafenamide (TAF), which was approved earlier this month as part of a combination HIV therapy, is a prodrug that breaks down into the active compound only after it sneaks inside white blood cells.
Within months, the company’s medicinal chemists had come up with a prodrug of a nucleoside inhibitor, now called GS-5734. The first studies in monkeys began in January 2015, and this spring the company and USAMRIID finally struck upon an effective dose.
But the program stalled over the summer. With cases of Ebola dropping, and the few remaining patients being funneled into the trial of the antibody cocktail ZMapp, Gilead had to wait for a way forward.
Then came the Scottish nurse. As has been widely reported, Pauline Cafferkey was “cured” in January of an Ebola infection she contracted while working in Sierra Leone. But last month her health started to deteriorate rapidly. The infection had roared back.
A relapse of the disease in a survivor is not unheard of. For example, a change in the color of aid worker Ian Crozier’s eyes alerted doctors to lingering viral particles in an area of the body that is tough for immune cells to reach. Other immune-privileged areas include the central nervous system and semen.
At the time that Cafferkey relapsed, healthy volunteers had safely received doses of Gilead’s drug of up to 150 mg. The same day it received a “compassionate use” request for GS-5734, Gilead sent the therapy to the London hospital where Cafferkey was being treated. She took the drug for 14 days and recovered.
“We can’t say that the drug helped her recover, but we can certainly speculate that it could have been part of it,” Lee says.
A small percentage of the more than 16,000 Ebola survivors in West Africa likely also have viral particles lingering in privileged areas. Some will eventually clear the virus on their own, but for those that relapse, doctors will need an antiviral that can access those hard-to-reach sites.
That population gives Gilead a possible route to approval for GS-5734. In addition to starting another study in healthy volunteers and completing studies in infected monkeys, Gilead is now planning a survivor cohort study in Africa. People will be treated for a short time—a week or two—and clinicians will check if the viral load in privileged sites has dropped.
Although FDA won’t comment on specific drugs, Cox agrees that this type of trial is viable. “If there are patients that have residual foci of infection in immunologically privileged sites, you could do a trial to evaluate the effects of an antiviral drug,” he says. “The provisos are that in any clinical trial there needs to be enough patients to gain enough experience with the product to draw valuable conclusions.”
That trial, along with Gilead’s monkey and healthy human data, would be enough to send GS-5734 to FDA for possible approval, Lee says. Although unlikely to be a moneymaker for Gilead, the drug would be eligible for a priority review voucher, an incentive for tropical disease drug development that allows the user to fast-forward the review of another medicine.
Gilead is confident enough in the drug’s chances that it is working on a manufacturing process and will have tens of thousands of vials available in the next few months, Lee says. The company, which has faced criticism for the price of its HIV and hepatitis C drugs, says it would make GS-5734 available cheaply if approved.
But the clock is ticking. A recent study of 93 men who survived Ebola shows that persistence of the virus drops over time: At two to three months, viral RNA could be detected in everyone; at six months, it was detectable in 65% of the men; at nine months, the figure dropped to 26%.
The drop “is a good thing but also means there’s a race if we’re going to do a study to look at eradicating the virus from persistent sites,” Bausch says.
THE NEXT THREAT
Also driving interest in the Gilead drug is the potential to use it against other RNA viruses. Gilead has tested its compound against Marburg and Sudan viruses as well as Middle East respiratory syndrome, or MERS. It has seen activity against all three in tissue cultures, according to Lee.

Indeed, researchers worry that with the focus on the Ebola virus, the world won’t be ready if the next big outbreak comes from another source—namely Marburg, Sudan, or MERS.
Advertisement
ZMapp, for example, is tailored to Ebola. And an antibody consortium that was established during the outbreak to find better cocktails also focused on Ebola. At this point, “antibodies are coming out of every crack of the universe for Ebola,” says Kartik Chandran, an immunologist at Albert Einstein College of Medicine.
Ebola researchers say some of the focus now should turn to antibodies for related viruses, or even a cocktail that is broadly protective against several RNA viruses. “For all we know, the next big outbreak will be caused by Marburg or Sudan, and ZMapp would be useless,” Chandran says. “The hope would be to have a Swiss Army knife cocktail that could hit all of them.”
Aside from antivirals such as Gilead’s, other drugs could also provide broad coverage. Chandran is trying to develop small molecules that target NPC1, the host protein the Ebola virus uses to enter human cells. Because other viruses also take advantage of that entry point, a drug against the target could have broad effect.
USAMRIID’s Bavari hopes that as his lab and others keep up the hunt for drugs for Ebola and other emerging threats, industry will stay on as a partner. “Two years ago, we couldn’t get a lot of industry to play with us,” he says. “Now, almost all the large pharmas are playing with us. We just have to make that more sustainable.”
That’s because although the threat of Ebola is waning, Bavari and other infectious disease experts know there will be a next time. “We don’t know when, we don’t know what,” FDA’s Cox says, “but we can predict that at some point in the future, we’ll see another emerging infectious disease.”




Join the conversation
Contact the reporter
Submit a Letter to the Editor for publication
Engage with us on Twitter