Advertisement
Grab your lab coat. Let's get started
Welcome!
Welcome!
Create an account below to get 6 C&EN articles per month, receive newsletters and more - all free.
It seems this is your first time logging in online. Please enter the following information to continue.
As an ACS member you automatically get access to this site. All we need is few more details to create your reading experience.
Not you? Sign in with a different account.
Not you? Sign in with a different account.
ERROR 1
ERROR 1
ERROR 2
ERROR 2
ERROR 2
ERROR 2
ERROR 2
Password and Confirm password must match.
If you have an ACS member number, please enter it here so we can link this account to your membership. (optional)
ERROR 2
ACS values your privacy. By submitting your information, you are gaining access to C&EN and subscribing to our weekly newsletter. We use the information you provide to make your reading experience better, and we will never sell your data to third party members.
Biological Chemistry
The fungus among us
Researchers race to study the human mycobiome and how it affects our health
by Sarah Everts
July 25, 2016
| A version of this story appeared in
Volume 94, Issue 30

By now, most of us have made peace with the fact that we are host to a complicated extended family of bacteria whose trillion-plus members give us vitamins, help us digest food, protect us from pathogens, and only rarely turn virulent on us. But what about the fungus among us?
“Wherever there are bacteria, there’s fungus as well,” says Mahmoud Ghannoum, a microbiologist at Case Western Reserve University. “If you just focus on bacteria, then you are ignoring an important part of the story.”
“Fungi have often been ignored,” adds Thomas Auchtung, who studies what he calls “phylogenetically underappreciated forms of life” at Baylor College of Medicine. “And because they’ve been totally ignored, we’re not sure how important they are.”
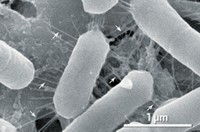
Auchtung and Ghannoum are part of a small community of researchers trying to untangle the role that fungi, a group that includes yeasts and molds, play alongside the larger population of bacteria living in and on our bodies. Although bacteria outnumber fungi by a thousand times, some scientists estimate there may be millions, and possibly billions, of fungi cohabiting our bodies.
Ghannoum says that many human microbiome studies have overlooked an essential part of the community, what many now call the mycobiome. In a recent commentary for The Scientist, Ghannoum did not mince words: “Clearly, the human mycobiome has an influence on both health and disease. The scientific community must adopt an all-inclusive characterization of the human microbiome going forward; studies that focus solely on bacteria are myopic and doomed to failure, and they squander precious research funds.”
Others in the field are a bit more circumspect. “Of course we had to start somewhere, so we started with bacteria,” says Mihai Netea, who studies both bacteria and fungi at Radboud Institute for Molecular Life Sciences. “We need research funding to do with the mycobiome what was done with the microbiome. We don’t even know what 1% of the mycobiome is doing,” he adds, in part because studying fungi is more challenging than studying bacteria.
Although it’s still early, those who are studying our fungal cohort have been finding tantalizing evidence that fungi may play a key role in health and our ability to withstand disease.
For example, last year, researchers in Spain found that certain fungi are more abundant in the guts of obese patients than in the guts of lean individuals (Sci. Rep. 2015, DOI: 10.1038/srep14600). Similar to what researchers have observed in the bacterial microbiome, the Spanish team also found there was less diversity of fungal species in the guts of obese people.
Likewise, scientists are finding that, compared with healthy people, individuals fighting HIV, cystic fibrosis, and inflammatory bowel disease have different fungal profiles in their mouths, lungs, and guts, respectively. These altered fungal populations are not just passive bystanders; they can sometimes worsen symptoms in already sick people. For example, when hepatitis B patients have an overabundance of certain fungi in their mycobiome—namely Candida and Saccharomyces—their symptoms are worse, Ghannoum notes.
“We are colonized by fungi every day, and most of the time it’s no problem,” Netea adds. “However, there are certain situations when fungi get opportunistic and pathogenic—often when we are harming our microbiome with antibiotics or when we are harming our immune system with chemotherapy or immunosuppressive drugs.”
Fungi for good and bad
In the past, most studies focused on the exploitative nature of these microorganisms. “We know a lot about pathogenic fungi” but much less about the fungi with which we live in harmony, Auchtung says.
For example, there’s been a lot of work studying Candida albicans, a common fungus found in and on humans that has a tendency to behave badly: It causes thrush in the mouth, yeast infections in the vaginal tract, and life-threatening invasions of the bloodstream. Researchers have also focused heavily on Candida parapsilosis. This common member of the human skin mycobiome kept a low profile for most of human history but has become increasingly infamous because it forms life-threatening biofilms on stents and catheters. “We didn’t evolve in an environment with stents and catheters,” Ghannoum says. “Now they are everywhere, and Candida parapsilosis loves adhering to them.”
Despite the overwhelming focus on harmful fungi, researchers examining the rest of the mycobiome are getting glimpses of the positive role played by previously overlooked organisms.

Consider members of the Pichia genus. Ghannoum found that in HIV patients who have Pichia species in their mouth, thrush-causing Candida fungi don’t flourish. He’s trying to identify and characterize the proteins secreted by Pichia that block germ tube formation in Candida, a first sign that Candida is turning virulent. Pichia is a long-standing favorite of apple growers, who spray it on apples to prevent other fungi from destroying their harvest. Ghannoum is interested in developing it as a fungal probiotic for humans.
Another fungus gaining fame as a good guy is Saccharomyces boulardii, whose populations increase when individuals eat certain types of fiber, such as the psyllium found in Metamucil and similar products. In clinical studies, researchers have found that the fungus has a protective effect against pathogens and helps the entire gut microbiome to stay in healthy equilibrium with the immune system. Preliminary work hints that S. boulardii probiotics might help combat several types of gastrointestinal disorders, such as antibiotic-associated diarrhea, Clostridium difficile infection, and Helicobacter pylori infection (Ther. Adv. Gastroenterol. 2012, DOI: 10.1177/1756283x11428502).

For some patients receiving bone marrow transplants, the mycobiome, along with its bacterial counterpart, appears to strongly influence long-term survival. Ying Taur at Memorial Sloan Kettering Cancer Center studies the gut microbiome and mycobiome of bone marrow transplant recipients receiving immune-suppressing drugs. The diversity of bacterial and fungal populations goes down in some patients, “with very dramatic clinical consequences,” Taur says. “Microbial diversity has a lot to do with whether transplant recipients are alive in three years. Diversity takes a dive as you undergo immune-suppression drugs.” The results hint that fungi, like bacteria, are a stable part of a healthy gut microbiome, he says.
Other researchers are finding that friendly fungi train our immune system to react to the bad guys. Over the past decade or two, researchers have identified receptors called dectins that are located on immune system cells called macrophages and monocytes. These receptors bind to β-glucan and other polysaccharides typically found on fungi and less often on bacteria. Sensing these polysaccharides is a way our immune system monitors fungi, explains Iliyan Iliev of Weill Cornell Medicine.
As a postdoc in David Underhill’s lab at Cedars-Sinai Medical Center in Los Angeles, Iliev studied inflammatory bowel disease in mice that had their dectin genes knocked out. They found that Candida tropicalis attacks the intestine of mice with no dectin. The already sick animals had increased gut inflammation and additional weight loss compared with controls, suggesting that a dectin fungal receptor might be an important player in the maintenance of a healthy gut mycobiome. The question is, how?
Netea and colleagues have observed that benign fungi can use the dectin receptor to train the immune system to respond to pathogens. When dectin receptors on macrophages of healthy individuals sensed benign Candida, epigenetic changes—such as histone methylation—took place in the genome of cells. The epigenetic reprogramming primed these macrophages to destroy pathogenic forms of Candida. “If a fungus interacts with a macrophage, the input stays for a long time,” Netea says, “giving the macrophage a very strong and enduring response.” This is one way beneficial fungi can prime, train, and strengthen the immune response to problematic fungi (Cell Host Microbe 2012, DOI: 10.1016/j.chom.2012.06.006).
Fungi are tricky to study
Scientists have caught these early glimpses of how the mycobiome might play a positive role in our bodies despite the many technical challenges facing those who wish to get to know our fungal cohort.
Like many members of the bacterial microbiome, a lot of the fungal species living in our bodies cannot easily be grown in the lab. Thus, researchers keen on understanding what these organisms are doing must instead directly sequence the fungal DNA found in a skin swab or stool sample and turn to genome databases to find out which organism the DNA belongs to. And therein lies a potpourri of problems.
For example, “fungi have very rigid cell walls,” Iliev says. “DNA isolation methods were designed for bacteria. They’ve needed to be modified just to be able to access fungal DNA.”
Meanwhile, the standard way to bar-code bacteria—using a component of their ribosome DNA called the 16S region—cannot be used to tell fungal species apart. So researchers have needed to find alternative regions of fungal genomes to use as bar coding. Their go-to standard is a component called the ITS—or internal transcribed spacer—region, which is found in the genome in between DNA coding for small-subunit ribosomal RNA and large-subunit ribosomal RNA.
Even with the right bar code, we don’t have the genome sequence information for many fungi, Auchtung says. Therefore, DNA sequences found in a sample don’t always match something in the database.
And even if you get a hit, there are a lot of discrepancies in fungal databases, in part because fungi lead such complex lives. Fungi often look completely different depending on their stage in life, so historically they’ve been incorrectly given different names, Auchtung explains. “Often we see that the same DNA matches to differently named organisms,” Iliev adds. “We constantly come across these problems.”
As researchers improve methods for studying the mycobiome, a clearer picture of the roles played by all organisms cohabiting our body awaits, Netea says.
“There’s no getting around the fact that bacteria are just a partial view. How many more answers can we get by sequencing our mycobiome?” Taur adds. “But then you also have to consider other minority members like archaea and viruses. It’s hard to know much about the things you’re not measuring,” he says. “Have we had blinders on the whole time? Have we realized yet how much the fungal counterparts can contribute to the story? It’s to be continued.”



Join the conversation
Contact the reporter
Submit a Letter to the Editor for publication
Engage with us on Twitter