Advertisement
Grab your lab coat. Let's get started
Welcome!
Welcome!
Create an account below to get 6 C&EN articles per month, receive newsletters and more - all free.
It seems this is your first time logging in online. Please enter the following information to continue.
As an ACS member you automatically get access to this site. All we need is few more details to create your reading experience.
Not you? Sign in with a different account.
Not you? Sign in with a different account.
ERROR 1
ERROR 1
ERROR 2
ERROR 2
ERROR 2
ERROR 2
ERROR 2
Password and Confirm password must match.
If you have an ACS member number, please enter it here so we can link this account to your membership. (optional)
ERROR 2
ACS values your privacy. By submitting your information, you are gaining access to C&EN and subscribing to our weekly newsletter. We use the information you provide to make your reading experience better, and we will never sell your data to third party members.
Infectious disease
Covid-19
How to interpret new studies on coronavirus variants
As new variants continue to pop up around the globe, here’s how to understand what the emerging research means for public health
by Laura Howes , Ryan Cross
August 31, 2021
| A version of this story appeared in
Volume 99, Issue 32

As SARS-CoV-2 proliferates into a Greek chorus of variants, headlines describing their risks raise fresh fears and resurrect old ones. Just a few months ago, people in countries fortunate enough to have ample supplies of COVID-19 vaccines were feeling as if the worst could soon be over. Now, the finish line seems to be moving further away.
Although scientists have learned much about the virus that causes COVID-19, SARS-CoV-2 is a moving target. Emerging variants mean researchers are continually reassessing how much of a threat the virus poses.
Support nonprofit science journalism
C&EN has made this story and all of its coverage of the coronavirus epidemic freely available during the outbreak to keep the public informed. To support us:
Donate Join Subscribe
To understand these new variants of the virus, scientists test them as they appear and compare them with the existing versions. Researchers are especially keen to answer two questions: Are neutralizing antibodies—previously produced by our immune systems in response to COVID-19 infection or vaccination—still able to stop the new variants from infecting our cells? And how readily do these variants spread compared with their predecessors? Over time, scientists can build a good model of how the variants behave, but as the process plays out in public, the differing findings or alarming headlines can become confusing.
As Ed Hutchinson a researcher at the MRC-University of Glasgow Centre for Virus Research puts it: “In the mayhem of the pandemic, vast amounts of information are being produced.” Much of that information is being shared on preprint servers and has not yet undergone peer review. So when a new study with potentially significant findings about a variant’s infectiousness or ability to evade our vaccines hits these servers, experts evaluate those data carefully.
C&EN spoke with a dozen scientists to understand how to respond to this changing landscape as we watch science happen in real time.

How do scientists in a lab study whether vaccination or a previous infection will protect us against a new variant?
Scientists use multiple types of lab tests to judge how well our immune systems will protect us from new variants. These tests typically involve taking antibodies from the plasma of people who are fully vaccinated or who recovered from COVID-19 and seeing how well they fight a new virus variant.
The simplest tests measure how well those antibodies bind to an isolated part of the coronavirus, such as the spike protein, which the virus uses to enter cells. Other tests gauge how well the antibodies prevent synthetic mimics of the coronavirus, called pseudoviruses, from infecting cells in a petri dish. The gold standard is to check how well the antibodies prevent live SARS-CoV-2 from infecting cells, but such experiments can be conducted only in high-security labs with strict safety protocols. “The process is laborious but not hard,” says Thomas Oguin III, who manages the virology unit that runs these studies at Duke University’s Regional Biocontainment Laboratory.
The lab tests that mix viruses and antibodies, called neutralization assays, help researchers predict if we have enough of the right kinds of antibodies to prevent infection. But what happens in the lab isn’t necessarily what will happen inside the body. “In order to make the assay work, we are simplifying the complexity of a natural infection enormously,” Hutchinson says. “But this is still really important because it means that we can make rapid and effective assessments of large numbers of variants quickly.”
What makes a variant more infectious, and how do scientists determine how infectious a new variant is?
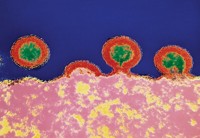
Viruses can evolve to be more infectious in several ways. Mutations in the coronavirus spike protein can give the virus a tighter grip on our cells, enabling a smaller amount of virus to start an infection. Other mutations may help the virus reproduce more quickly or in greater quantities, increasing the chance that an infected person will spread the virus to someone else.
A more infectious virus doesn’t necessarily make people sicker, but it does infect more people, making outbreaks harder to control. That’s what we’re seeing with Delta, says Priyamvada Acharya, a researcher at the Duke Human Vaccine Institute. Neutralizing antibodies still stop that variant, albeit not as well as the original virus. But Delta’s boost in how easily it can spread and infect someone is driving the increase in case numbers and breakthrough infections in vaccinated people.
In fact, Delta spreads more easily than Beta, even though neutralization assays show that the Beta variant is better at evading our neutralizing antibodies than the Delta variant.
In the lab, researchers can mix a live virus or pseudovirus with cells to measure how much virus is needed to infect cells or how quickly the virus replicates. Scientists can also expose animals like ferrets to the virus to measure this. But the real world has lots of confounding factors, including how people are interacting day to day. A variant that evades the immune response but isn’t very transmissible might just die out, says Robert Seder, an immunologist at the National Institutes of Health’s National Institute of Allergy and Infectious Diseases (NIAID). Epidemiologists and modelers use population-level data to calculate the R0 number, which indicates how many people on average each infected person will infect. The original SARS-CoV-2 virus was calculated as having an R0 of around 2–3 in unvaccinated people who made no changes to their behavior to try and stop transmission. The Delta variant is calculated to be about 6–7 under the same conditions.
“The worst-case scenario,” Seder says, is a variant that can spread as well as Delta and be really good at evading the immune system. “We are not there yet, but we are monitoring that very closely.”
What do experts suggest looking for when research comes out about a new SARS-CoV-2 variant, especially when it hasn’t been peer-reviewed?
Preprints that examine the variants often have scary claims, but these should be interpreted cautiously.
“When I look at a preprint, I am looking at the numbers,” says Miles Davenport, head of the Infection Analytics Program at the University of New South Wales in Sydney. “I don’t pay very much attention to the claims because sometimes the claims in an abstract or discussion don’t actually match what the data show.” Davenport focuses on a few key points: the kind of neutralization assay the researchers used, where their antibody samples came from, how they collected data on vaccine efficacy, and how the researchers defined mild or severe disease.
Those neutralization assays often suggest that our antibodies are better at stopping the original virus than the variants, but the magnitude of any change is important. For example, a 2-fold reduction—meaning a 50% drop—in antibodies that neutralize the virus might not be a problem, but a larger 10-fold or 100-fold reduction—a 90% or 99% drop—might be, according to Rachel M. Presti, who directs the Infectious Disease Clinical Research Unit at Washington University School of Medicine. And every person has a different antibody response to vaccination: if your immune system has a lot of antibodies, a 50% decrease in neutralization probably isn’t a problem, Presti says. But if your antibody levels are low, it could be enough to give the virus the upper hand.
Researchers also suggest looking at whether a paper analyzes multiple variants head to head. It is trickier to compare numbers between papers because different labs use different assays, different sources of antibodies, different virus models, and different ways to calculate metrics like neutralization effectiveness, says Steve Kemp, who researches infectious diseases at University College London. These can all contribute to groups reporting different numbers for the same variant.
The most important takeaway, Kemp says, is that different experiments often point in the same direction. Pay attention when multiple groups are finding that neutralizing antibodies don’t work quite as well against a variant, even if the numbers they report differ.
For papers discussing whether vaccines will be less protective against a variant, it’s also important to look at what, exactly, the authors mean by vaccine effectiveness. Protecting against mild infection is a higher bar than preventing severe disease, hospitalizations, and death. And it is still hard to predict from a lab test exactly how effective a vaccine will be at each of those tasks.
We’re hearing a lot about infections in vaccinated individuals. Does this mean the vaccines aren’t working?
No. The number 1 goal of the COVID-19 vaccines is to prevent severe disease and death. By that measure, the shots are by and large still a success, Presti says. But the variants may force us to reset our expectations for what the vaccines can do. “Very few vaccines completely block infection,” Presti says. As variants evolve to be more infectious and partially evade our antibody responses, mild infections may become more common.
Right now, groups around the world are trying to use real-world data to assess how well the vaccines are working against Delta. The results have been mixed depending on the vaccine and location. One study in the UK found that two doses of the Pfizer vaccine were 88% effective in preventing symptomatic disease with Delta, while two doses of the AstraZeneca vaccine were 67% effective. And in July, when the Delta variant was the predominant strain in Minnesota, the Mayo Clinic found that the Pfizer vaccine was only 75% effective at preventing hospitalization, according to a recent preprint.
Scientists are also working to understand the type of immune response a vaccine needs to elicit to offer robust protection—what the field calls “immune correlates of protection”—to better predict how well vaccines will work against new variants.
Davenport’s group in Sydney has shown that the efficacy of seven COVID-19 vaccines correlates with levels of neutralizing antibodies that the shots induce and that the best protection comes from messenger RNA (mRNA) vaccines. And David Benkeser, a biostatistician at Emory University, helped analyze data from the clinical trial of Moderna’s mRNA vaccine and found that people with the most neutralizing antibodies were the least likely to test positive for COVID-19.
Those studies are a step toward defining the quantity of antibodies needed to prevent a particular percentage of COVID-19 cases, but Benkeser cautions that those numbers could change with each variant. “Risk should be thought of as a continually shifting measure,” he says. For now, Benkeser is encouraged by the high levels of neutralizing antibodies induced in most people who get the mRNA vaccines, which he thinks provides significant “wiggle room” for dealing with variants.
Will we need booster shots to protect us from the variants?
For healthy, fully vaccinated people, a mild infection with Delta could act as a natural boost to our immunity against the coronavirus, Seder says. But for immunocompromised people and older adults who typically don’t produce a lot of antibodies, booster shots could be key to prodding their immune systems to better protect them from severe disease.
In a preprint, Seder’s team at NIAID shows that a booster dose of Moderna’s vaccine given to monkeys 6 months after their initial shots increased neutralizing antibody levels 7-21 times. When the monkeys that received the booster were challenged with a Beta infection 8 weeks later, they were protected from infection in their upper and lower airways. Although there are no published data on boosters in humans yet, Seder thinks boosters will be key for people too. “For older people and at-risk groups, boosting is a no-brainer.”
Advertisement
Several countries have recently authorized booster shots of the mRNA vaccines for immunocompromised people, while others, like the US and Israel, are rolling out boosters more broadly. “I think it will help reduce hospitalizations with vaccinated individuals,” says Mehul Suthar, a researcher at the Emory Vaccine Center. But he stresses that even with a booster, people may still get a mild infection. Like the original shots, the goal of boosters is to prevent severe disease.
Researchers say that if the virus mutates to the point where the existing vaccines no longer protect people from severe disease, mRNA vaccine technology will likely provide the quickest way to make new shots tailored to future variants. In fact, several vaccine makers are already working on new versions based on the Beta and Delta variants. But with many people worldwide still waiting for their first shots, some researchers are questioning the wisdom of broadly distributed boosters. “At this moment I think there is going to be more bang for your buck in getting an unvaccinated person a vaccine than giving a vaccinated person a booster,” Benkeser says.
Why don’t scientists have clearer answers?
There’s variability in how virus variants respond to human antibodies in the lab, and the real world is much more complicated than a simple assay can reflect. How infections play out in communities depends on the number of people vaccinated in a given region, the behavior of those people, and many other factors. But while the details differ, most scientists agree on the main points about how the virus works and how we can best end the pandemic.
Many scientists think that SARS-CoV-2 is here to stay. “We are not going to eradicate coronavirus. It is going to continue to circulate, and the evidence suggests that people will be susceptible to reinfection,” Davenport says. But being vaccinated can help us ward off future encounters with the virus. We might still get sick, and the virus could still cause serious problems for people who are not able to mount a strong immune response, but over time, COVID-19 could morph into more of a seasonal nuisance than a public health emergency.
“Get vaccinated,” Benkeser says. “Don’t let fear of variants deter you from getting a highly safe and effective vaccine.”




Join the conversation
Contact the reporter
Submit a Letter to the Editor for publication
Engage with us on Twitter