Advertisement
Grab your lab coat. Let's get started
Welcome!
Welcome!
Create an account below to get 6 C&EN articles per month, receive newsletters and more - all free.
It seems this is your first time logging in online. Please enter the following information to continue.
As an ACS member you automatically get access to this site. All we need is few more details to create your reading experience.
Not you? Sign in with a different account.
Not you? Sign in with a different account.
ERROR 1
ERROR 1
ERROR 2
ERROR 2
ERROR 2
ERROR 2
ERROR 2
Password and Confirm password must match.
If you have an ACS member number, please enter it here so we can link this account to your membership. (optional)
ERROR 2
ACS values your privacy. By submitting your information, you are gaining access to C&EN and subscribing to our weekly newsletter. We use the information you provide to make your reading experience better, and we will never sell your data to third party members.
Diagnostics
Assay detects latent tuberculosis
Biomarker signatures could help doctors assess a patient’s risk of dormant bacteria waking up again
by Celia Henry Arnaud
February 13, 2019
| A version of this story appeared in
Volume 97, Issue 7

Nearly a quarter of the world’s population has latent tuberculosis infection (LTBI). These people don’t have symptoms of the infection because the TB bacteria living inside them are dormant. In about 10% of those people, the bacteria will wake up, but diagnosing latent TB and predicting who is at risk for reactivating is hard.
A team led by Ryan C. Bailey of the University of Michigan and Patricio Escalante of Mayo Clinic reports an assay that reveals diagnostic signatures that doctors could use to both diagnose latent TB and evaluate a patient’s reactivation risk (Integr. Biol. 2019, DOI: 10.1093/intbio/zyz001).
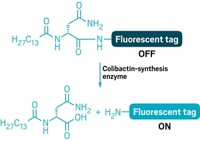
The assay provides information about how immune cells in a patient respond to threats. Some of these responses may indiciate increased risk of reactivation.
To get information about these responses, the researchers use arrays of microring resonators to detect proteins secreted by mononuclear blood cells—a type of immune cell—in response to antigens related or unrelated to TB. When antibodies on the resonator surface bind a secreted protein, the refractive index of the device changes, producing a shift in the device’s optical readouts. The researchers exposed immune cells from 50 people with LTBI to five substances: TB-specific peptides, the protein derivative used in the tuberculin skin test, the yeast Candida albicans, and positive and negative controls.
“By testing cells' secretion patterns that have nothing to do with TB, we’re actually monitoring basal immune function,” Bailey says. By subtracting the responses to the non-TB substances from the TB ones, they revealed signatures specific to different states of LTBI. “We saw almost three times as many biomarkers that correlated with different TB states,” Bailey says.
“LTBI is a really hard problem,” says Brian M. Paegel, a scientist at Scripps Research’s Florida campus who works on diagnostic technology development. The researchers behind the new study “are taking it to a new level. They’re looking at a cellular response to the presence of those antigens, providing a potentially richer data set to tease out the presence of LTBI.”
But first the researchers need to study more TB patients. “To further validate this biomarker signature we are working with a TB clinic in Tijuana, where TB prevalence and reactivation rates are much higher than the US,” Bailey says.


Join the conversation
Contact the reporter
Submit a Letter to the Editor for publication
Engage with us on Twitter