Advertisement
Grab your lab coat. Let's get started
Welcome!
Welcome!
Create an account below to get 6 C&EN articles per month, receive newsletters and more - all free.
It seems this is your first time logging in online. Please enter the following information to continue.
As an ACS member you automatically get access to this site. All we need is few more details to create your reading experience.
Not you? Sign in with a different account.
Not you? Sign in with a different account.
ERROR 1
ERROR 1
ERROR 2
ERROR 2
ERROR 2
ERROR 2
ERROR 2
Password and Confirm password must match.
If you have an ACS member number, please enter it here so we can link this account to your membership. (optional)
ERROR 2
ACS values your privacy. By submitting your information, you are gaining access to C&EN and subscribing to our weekly newsletter. We use the information you provide to make your reading experience better, and we will never sell your data to third party members.
Pharmaceuticals
Drugs for Diabetes
New therapies targeting hormone in the gut promise more benefits than existing drugs and show potential for regenerating beta cells
by LOUISA WRAY DALTON, C&EN WASHINGTON
October 25, 2004
| A version of this story appeared in
Volume 82, Issue 43

Diabetes is not easy to treat, but new experimental therapies are raising hopes that better options for managing this disease will become available in the near future. The new therapies center on a little-known player in the elaborate process of human food digestion: the 30-amino-acid peptide hormone known as glucagon-like peptide 1 (GLP-1).
A hallmark of diabetes is an abnormally high level of glucose in the blood, a condition known as hyperglycemia. Since the 1920s, patients have depended on injections of insulin to help keep glucose in check. Insulin does this by preparing cells to admit the sugar.
A healthy body secretes only as much insulin as is needed to keep blood sugar levels steady. But in a patient with diabetes, the body either produces little or no insulin (type 1 diabetes and often late-stage type 2 diabetes) or doesn't respond adequately to the insulin it has (type 2 diabetes). Insulin injections, as well as insulin-sensitizing drugs, which increase a diabetic's response to insulin, extend lives by bringing down skyrocketing blood glucose levels.
Although hailed as a miracle cure for diabetes, insulin doesn't actually cure the disease for roughly 18 million patients with diabetes in the U.S. Neither is it a gentle treatment. Along with many insulin-sensitizing drugs, it encourages weight gain. Moreover, take too much insulin at once and you can find yourself in the dangerous state of hypoglycemia, where the brain is not getting enough glucose. Many diabetic patients on insulin therapy tend to keep their sugar levels a bit high just to avoid hypoglycemia.
The complexity of insulin therapy is part of what's driving the search for new treatments. Another driver is the growing body of knowledge that is revealing targets for pharmaceuticals that may be more manageable than insulin. Furthermore, no pill or injection to date addresses the problem of dying pancreatic beta cells, a fundamental dysfunction seen in diabetes.
BETA CELLS, located in the islets of the pancreas, are the only cells in the body that produce and secrete insulin. In type 1 diabetes, previously called juvenile diabetes, immune cells actually attack and kill the beta cells. Those with type 2 diabetes, previously called adult-onset diabetes, start out with working beta cells, but over time, as insulin demand increases because of decreased sensitivity to insulin, the overworked beta cells eventually stop replacing themselves. As yet, no drugs stop or reverse the progression of type 2 diabetes.
That may soon change. In 2005, Amylin Pharmaceuticals hopes to launch a diabetes therapy built on a new treatment paradigm based on GLP-1. The drug is intended to manage blood glucose levels while encouraging weight loss and avoiding the risk of hypoglycemia. But what may be most significant is that the treatment has the unique and remarkable potential to restore and protect failing beta cells.
Exenatide, as Amylin's drug is called, is not alone. It is just the first of its kind. Almost every major and many smaller pharmaceutical firms have a drug in the pipeline that affects the same biochemical pathway that Exenatide does.
In response to a meal, endocrine cells in the small intestine called L cells release GLP-1. In turn, GLP-1 prepares the body for the inevitable glucose surge, producing what is called an incretin effect. GLP-1 stimulates the release of insulin from pancreatic beta cells as long as blood glucose levels are high. It also inhibits the release of the hormone glucagon--which controls release of glucose from the liver--from the pancreas, so the liver stops dumping glucose into the bloodstream. Moreover, GLP-1 slows the emptying of the stomach, leading to a feeling of fullness and discouraging more food intake.
GLP-1 works through a specific GLP-1 receptor in the beta cell of the pancreas, leading to insulin release. However, how it mediates all of its effects is not entirely worked out. Many suspect that the nervous system is involved. Shortly after GLP-1 is released from the L cells, it encounters neurons in the gut. These may transport GLP-1 signals to the brain with messages of satiation.
GLP-1 was isolated decades ago as one of the products of the proglucagon gene. Joel F. Habener, professor of medicine at Harvard Medical School, and his group; a group at the University of Copenhagen led by physiology professor Jens Juul Holst; and others recognized its effect on insulin release in the 1980s. "Finally in 1992," Holst says, "we and some Swedish workers found that GLP-1 had these fabulous activities in type 2 diabetic patients," primarily insulin stimulation and the control of high blood glucose. "From then on, we knew that this had a huge potential in diabetes treatment."
A VERY ATTRACTIVE aspect of GLP-1's activity is that it stimulates insulin release only so long as there is enough glucose to warrant it. It's glucose-dependent. Thus a drug that mimics GLP-1's activities could help manage high glucose levels without running the risk of inducing hypoglycemia. However, GLP-1 itself cannot be a practical drug. It's an easily digestible peptide with an extraordinarily short half-life of 90 seconds. As soon as the possibility of GLP-1-based therapy became known, a few drug companies began searching for molecules that could mimic the action of GLP-1 but would last a good deal longer.
In the meantime, Holst and some coworkers decided to find out if the GLP-1 incretin effect was one that could last over the long term. Short-term infusions of GLP-1 made a difference. But what about over weeks? "Will it work? Will the benefits wane over time? Will there be side effects?" Holst remembers asking as they set up the study. If GLP-1 itself couldn't have a sustained effect, he and his colleagues reasoned, neither could a longer lasting mimic. Their results, published in Lancet in 2002, were striking. They found that a therapy based on GLP-1 was far more promising than most had realized.
Holst's group administered GLP-1 or saline continuously to 20 patients with type 2 diabetes for a period of six weeks. By keeping the dose sufficiently low, they avoided the biggest side effect of GLP-1 therapy: nausea and vomiting.

Furthermore, the patients felt less hungry and steadily lost weight (with an average loss of 4.2 lb). No drug for the treatment of diabetes had ever shown such a side benefit. Scientists believe the weight loss is due to GLP-1's ability to suppress appetite and slow gastric emptying.
Finally, the data suggested that continuous GLP-1 therapy improved the function of pancreatic beta cells. Changes in beta cells are difficult to study in human clinical trials. But the pancreas of animals with diabetes can be observed directly. And in the pancreas of rats and mice, GLP-1 is said to work like a vitamin on the beta cell. It stimulates insulin secretion and insulin biosynthesis. It increases the genesis of new beta cells and their proliferation and differentiation. And it inhibits the programmed death of beta cells.
At the end of the 2002 Lancet study, "the weight loss, the hemoglobin A1C drop, the improvement in insulin sensitivity, the improvement in beta cell function ... everything was there, really," Holst says. "We were confident from then on that a therapy for diabetes based on GLP-1 would be feasible."
Many researchers agreed with Holst, and the race to get a GLP-1-based drug to the market turned into a sprint.
Amylin Pharmaceuticals, the company that will likely be first to market with a therapy in 2005, has taken the most unusual tack. Its drug is a peptide found in the saliva of the Gila monster. "It is the first endocrine hormone from salivary glands that has glucoregulatory action," says Soumitra S. Ghosh, senior director of research chemistry at Amylin.
John Eng, an endocrinologist at the Bronx Veteran's Affairs Medical Center, New York City, first found the peptide. In the 1990s, he was searching for bioactive peptide hormones in lizard venoms. He came across exendin-4, a 39-residue peptide that binds to the GLP-1 receptor in vitro. He subsequently established that the molecule lowers blood glucose levels in a diabetic mouse model. An Amylin scientist who saw a presentation of Eng's work recognized the potential of the molecule for its glucose-lowering action. Eng holds the patent on the use of exendin-4, and Amylin licenses the patent. Amylin's synthetic version is called Exenatide.
Exenatide shares 53% of its amino-acid sequence with GLP-1. Like GLP-1, exendin-4 is broken down by peptidases, but more slowly. It has a two- to four-hour half-life when injected subcutaneously and is eventually cleared by the kidneys. For this reason, Exenatide must be injected twice a day.
Exenatide is remarkably well tolerated by humans. Because it is foreign, the peptide elicits some antibodies in some patients, Ghosh says. However, the antibodies have no effect on glycemic control of Exenatide, he explains.
Although it appears that several of the effects of Exenatide may be mediated through the GLP-1 receptor, researchers can't be sure that all are, Ghosh says. Clinical studies show that Exenatide stimulates insulin in a glucose-dependent manner just as GLP-1 does. It slows gastric emptying and inhibits the secretion of glucagon. Patients lose weight. And in animals, Exenatide slows the dying of existing beta cells while stimulating the differentiation and production of new ones.
One other company, Novo Nordisk, has a GLP-1 analog entering Phase III clinical trials this year. Called liraglutide, the candidate is a modified GLP-1. Novo Nordisk added a 16-carbon fatty acid to a lysine near the middle of the peptide chain of GLP-1. Once the drug is in the bloodstream, the fatty acid portion binds to serum albumin, the plasma transport protein. GLP-1's piggybacking on the serum albumin extends the lifetime of GLP-1. Thus, liraglutide's half-life is long enough that it needs to be injected just once a day. The piggybacking also distributes GLP-1 throughout the body. Serum albumin continuously releases the peptide, leading to a stable level.
At least two other companies have GLP-1 peptide analogs in clinical testing. Zealand Pharma has developed ZP-10, a modified GLP-1 peptide with a tail of lysines at the N-terminus. And Conjuchem is producing a GLP-1 analog bound to the protein albumin to help extend the drug's half-life.
The primary drawback of all of these drugs is that they must be injected, because peptides are difficult to formulate into oral drugs. On top of that, they can cause nausea, especially at first. Many patients get used to it after a day or two. However, the fact that these drugs can induce nausea likely underscores that they are powerful enough to affect body weight. GLP-1 analogs can raise and sustain physiological levels of GLP-1 higher than their normal level for 24 hours a day, and some researchers speculate that that may be what it takes to suppress appetite and shed pounds. Damping appetite may require such a sustained effect. Otherwise, people might just run out and eat chocolate between meals.
Still, it's asking a lot of diabetic patients to inject a drug that might make them nauseous when they don't feel sick, comments Thomas Hughes, global head of diabetes at Novartis Institutes for Biomedical Research.
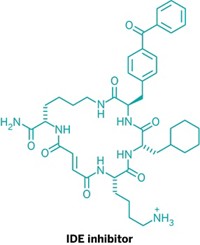
Novartis has led the race in developing a GLP-1-based therapy that comes in pill form and doesn't make one feel sick. That development goes back to the mid-1990s, when several research groups, including that of Holst and Carolyn F. Deacon at the University of Copenhagen, discovered what inactivates GLP-1 so quickly.
Once GLP-1 diffuses from the L cells to the intestinal capillaries, it encounters the enzyme dipeptidyl peptidase IV. DPP-IV promptly snips two amino acids off GLP-1's N-terminus and inactivates the hormone. Only a quarter of active GLP-1 molecules make it as far as the liver, where they again encounter DPP-IV. "So only about 10% of what is secreted actually makes it to the systemic circulation. That is very little," Holst says.
The discovery prompted many pharmaceutical firms to start looking for a small molecule to inhibit DPP-IV. "Fourteen companies at last count," Habener says. The goal is popular because the market for effective oral drugs to treat diabetes is big. More than half of the patients with diabetes in the U.S. take oral medication only.
Advertisement
But pursuing DPP-IV inhibition has its risks. DPP-IV is by no means a one-substrate enzyme. It clips off the end of many proteins that have an alanine or proline at the second position. The "very surgically precise excision of two amino acids," as Habener describes the action of DPP-IV, inactivates some substrates, such as GLP-1, but activates others, such as some neuropeptides and molecules important in activating white blood cells of the immune system. For a long time, in fact, immunologists knew DPP-IV by a different name: CD-26.
FURTHERMORE, that DPP-IV is active in the immune system gives therapy based on DPP-IV inhibition a theoretical safety issue that has been hanging over the field. Only when the long-term safety is established will the issue be completely laid to rest.
To find a candidate based on DPP-IV inhibition, Novartis took a dipeptide template--valine pyrrolidide--that fits into DPP-IV's active site and searched for small molecules with similar shapes.
This summer, Novartis released Phase II clinical data on their leading compound, LAF-237. The results "sort of astonished a lot of us. The DPP-IV inhibitor has few side effects and almost all the benefits you want," Habener says, "despite the fact that DPP-IV is involved with the activation of other neuropeptides and [molecules of the immune system]."
"Not even we, who had worked closely with these substances for a long time, thought that they would be as effective as they are," Holst agrees.
For one year, a group of patients in Europe with type 2 diabetes took LAF-237 in combination with metformin, a conventional diabetes drug. Clear deterioration of glycemic control was observed in the control group, which took only metformin, but not in the LAF-237 group. At the end of the study, patients on the combined therapy displayed hemoglobin A1C levels that were 1.1% lower than those on metformin alone. Beta cell markers improved and glucagon secretion went down. Moreover, the patients gained no weight, and their cholesterol levels even dropped slightly.
Treating patients with a DPP-IV inhibitor differs in some significant ways from treating with GLP-1 agonists. The patients don't experience nausea. Nor do they lose weight. Novartis didn't expect weight loss because their animal studies did not show decreased food intake or weight loss and only a weak slowing of gastric motility. But weight neutrality, Hughes points out, "is in fact a very positive feature--given that most antidiabetic agents actually lead to significant weight gain."
Why doesn't LAF-237 affect weight? Some researchers surmise that a DPP-IV inhibitor does not reduce appetite because it cannot raise the level of GLP-1 above its natural level.
As for beta cell protection, most researchers say it remains to be seen whether DPP-IV inhibitors will help restore the pancreas. "The literature on DPP-IV inhibitors is really scanty" regarding beta cell protection, Holst points out.
Novartis' Hughes says that animals treated with LAF-237 do show a preservation of beta cells. Histological evaluation of the animal's pancreas after chronic exposure shows increased staining of insulin, increased expression of key proteins involved in beta cell function, and improved function of the islets of the pancreas, he notes.
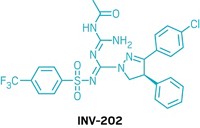
OTHER COMPANIES are on Novartis' tail. Merck has a DPP-IV inhibitor called MK-0431 in clinical trials. Merck scientists emphasize that specificity is crucial for DPP-IV inhibition. Earlier compounds they had tested also inhibited enzymes related to DPP-IV and were profoundly toxic.
Bristol-Myers Squibb has developed a compound, called BMS-477188, that "fits very nicely into the enzyme active site" of DPP-IV, says Lawrence G. Hamann, a research chemist there. The Phase II clinical data show it is a potent high-affinity inhibitor.
GlaxoSmithKline has moved its candidate, GSK23A, into clinical development. In August, researchers from Hoffmann-La Roche and Eisai talked about promising DPP-IV inhibitors at the American Chemical Society national meeting in Philadelphia. And a crowd of other companies is actively searching for new DPP-IV inhibitors.
Many of the most promising inhibitors sport an -aminoacylpyrrolidine backbone that fits well into DPP-IV's active site. Crystal structures of DPP-IV's active site, solved by several laboratories in 2003, reveal why. A glutamate in the enzyme's active site forms a salt bridge with the basic amine; an arginine stabilizes the amide carbonyl; and the drug's proline ring fits into a tight pocket of hydrophobic and aromatic side chains.
Regarding side effects of DPP-IV inhibitors, Holst says there shouldn't be any, and the clinical data for LAF-237 seem to support him. But why would inhibiting an enzyme that cleaves so many substrates and may have important functions in the immune system have so few consequences?
Hughes has a theory. He thinks DPP-IV is primarily a protein-scavenging enzyme, not a glucose regulator. It cleaves proteins so that the body can retain the amino acids. "Evolutionarily, this was probably a very significant function," Hughes says. For wild animals or early humans who had a limited amount of protein in their diets, helping the body digest every amino acid was important. But in today's protein-rich diets, losing a few amino acids doesn't matter. And the fact that DPP-IV degrades other peptide hormones suggests it is not involved in regulation. It's really more an accident, he believes, that DPP-IV happens to be the primary peptidase for GLP-1. For all of DPP-IV's other substrates, additional peptidases fill in.
As evidence to support his theory, Hughes says that GLP-1 secretion is regulated by a feedback loop that depends on levels of GLP-1 and not on DPP-IV activity. In addition, rats and mice that don't express the DPP-IV gene--called knockouts--are "overwhelmingly normal."
"They are viable," Holst says. "They eat as much as normal mice. They grow as much. They breed as well. The message from the knockout mouse is that DPP-IV is not a super vital system."
Nor are the DPP-IV knockout rodents immune-compromised, suggesting that the role DPP-IV plays in the immune system is either readily replaced or not essential. Curt D. Haffner at GlaxoSmithKline points out that, because diabetes likely involves an inflammatory component, inhibiting DPP-IV's immune function might actually be a boon to the patient.
Although GLP-1 analogs and DPP-IV inhibitors offer similar benefits for patients with diabetes, the drugs may inhabit very different niches of the diabetes market.
DPP-IV inhibitors are expected to compete with oral drugs such as sulfonylureas and metformin. They could be recommended for early-stage or even prediabetes to help manage hyperglycemia right from the start. And as Novartis has already illustrated, DPP-IV inhibitors may be used in combination with the other families of diabetes drugs.
GLP-1 agonists and peptides similar to GLP-1, because they must be injected, will likely compete with other injected compounds used in later stage diabetes. They will be another tool to help avoid last-resort insulin therapy, and may even replace insulin entirely in some type 2 patients.
"Type 2 diabetic patients who have been on insulin therapy for a long time can be treated with GLP-1-based therapy," Holst says. "It works beautifully in these patients." Its advantages are that the patient would lose weight and avoid the risk of hypoglycemia at the same time.
Finally, Habener says, if GLP-1-based therapies do truly regenerate beta cells, they will be used for every stage and for both types of diabetes to restore the dying islets of the pancreas.
Holst illustrates the significance of such a therapy by describing one of the most comprehensive and longest running diabetes studies to date. The U.K. prospective diabetes study followed a large number of type 2 diabetic subjects in England for 10 years or more, he says. Most were on some type of conventional therapy: metformin, insulin, sulfonylureas, or a combination.
"It was very clear that after a short period of improvement in metabolic control, all of the patients, regardless of therapy, showed a linear impairment in metabolic control. It got worse and worse and worse. And none of the therapies had any efficacy after some years, including insulin therapy," Holst says. "This is a terribly dramatic finding. It must be concluded today that all of these conventional therapies are really without long-term effect--that they will show inefficiency in the long run. Now, GLP-1 and all of the GLP-1-based therapies show they have this tremendous potential of perhaps being able to rescue the endocrine pancreas of a diabetic subject. Because of this, it may be able to halt the progression of the disease. That's why people are so enthusiastic about GLP-1."






Join the conversation
Contact the reporter
Submit a Letter to the Editor for publication
Engage with us on Twitter