Advertisement
Grab your lab coat. Let's get started
Welcome!
Welcome!
Create an account below to get 6 C&EN articles per month, receive newsletters and more - all free.
It seems this is your first time logging in online. Please enter the following information to continue.
As an ACS member you automatically get access to this site. All we need is few more details to create your reading experience.
Not you? Sign in with a different account.
Not you? Sign in with a different account.
ERROR 1
ERROR 1
ERROR 2
ERROR 2
ERROR 2
ERROR 2
ERROR 2
Password and Confirm password must match.
If you have an ACS member number, please enter it here so we can link this account to your membership. (optional)
ERROR 2
ACS values your privacy. By submitting your information, you are gaining access to C&EN and subscribing to our weekly newsletter. We use the information you provide to make your reading experience better, and we will never sell your data to third party members.
Biological Chemistry
Social Reassessment, Regulation, and Growth: 1960-80
June 20, 2005
| A version of this story appeared in
Volume 83, Issue 25

COVER STORY
SOCIAL REASSESSMENT, REGULATION, AND GROWTH: 1960-80
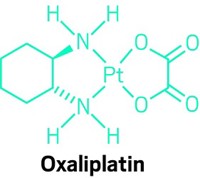
The pharmaceutical industry was buffeted by significant scientific, medical, political, and market forces between 1960 and 1980. Approaches to drug discovery and early-stage testing changed as medical advances made it possible to identify compounds that block specific physiological processes. Major innovations were made in cardiovascular drugs (starting with antihypertensives and beta-blockers in the 1960s, followed by calcium-channel blockers, ACE inhibitors, and cholesterol-reducing drugs in the 1970s and 1980s); tranquilizers, antidepressants, and antihistamines with fewer side effects; nonsteroidal anti-inflammatory drugs; oral contraceptives; cancer therapies; and means of controlling the symptoms of Parkinson's disease and asthma attacks. Clinical testing achieved greater standardization under strict FDA oversight in the U.S., whereas many European and other countries maintained more flexible systems that allowed drugs on the market sooner, contingent on closer physician monitoring of side effects. As a result, a hotly contested "drug lag" motivated U.S.-based firms to diversify into fragrances, cosmetics, and other consumer products.
Though chemists at least from the days of Ehrlich had hoped to design medicines to fit molecular targets, so-called rational design became a real possibility in the 1970s. In rational design, substrates or receptors for enzymes, hormones, or neurotransmitters known to be involved in a particular disease are selected on the basis of knowledge of the body's biochemical and physiological processes. Next, chemists investigate compounds that might block the function of the chosen target molecule. Alternatively, or simultaneously, a search is done among natural sources, including substances produced by microbes that might have the desired biochemical effect. Drawing on the store of molecular structure-activity relationships that chemists have built up over time, researchers modify the lead candidate from this process to turn it into a pill or injection tolerated by humans. While rational in intent, the process to this day often benefits from sheer chance and the tenacity of researchers who develop a passionate attachment to certain molecules, such as Miguel A. Ondetti and Emily Soba with the ACE inhibitor succinyl-L-proline, which was developed into captopril, or Albert Carr with a metabolite of terfenadine, which was marketed as an antihistamine.
During the 1960s and '70s, new instruments were brought to bear on the process of drug discovery, including nuclear magnetic resonance and high-pressure liquid chromatography. Rendering the pharmaceutical laboratory yet more dry, computers were increasingly used to perform complex calculations such as Fourier transforms and to host databases used in comparing new compounds to established reference molecules and in analyzing results from large clinical trials.
Among the factors driving adoption of new instruments and computers was a major new regulatory law. Starting in the late 1950s, the pharmaceutical industry faced a lengthy investigation into pricing policies and marketing approaches spearheaded by former Sen. Estes Kefauver (D-Tenn.). Kefauver brought to public attention huge markups between raw material costs and the final price of a drug; his congressional hearings also exposed a variety of unsavory marketing practices.
Nearly simultaneous with the Kefauver investigation in the U.S., the thalidomide tragedy--a case in which a sedative widely marketed in Europe, South America, and parts of Asia caused severe birth defects in approximately 10,000 children worldwide--drew attention to inadequate clinical testing and regulatory oversight prior to the marketing of new drugs. In Germany, home to the manufacturer (Chemie Grnenthal) and the country hardest hit by the tragedy, a 1961 statute ordering federal registration of new medicines was strengthened in 1964 to require prescription drug status for new drugs. Nevertheless, a more comprehensive drug law with formal premarket requirements for drug safety and efficacy was not enacted in Germany until 1976.
In the U.K., the Ministry of Health responded to the crisis by establishing the Committee on Safety of Drugs (CSD) in 1963. Although it worked closely with the government, CSD was not a regulatory agency and did not police physician or industry behavior before or during clinical trials. A national licensing authority was established in the 1968 Medicines Act, which put the control of market access for new drugs under the Committee on Safety of Medicines.
Although thalidomide was not marketed in the U.S., publicity about birth defects in Europe led Congress to rapidly pass new legislation. Whereas Kefauver had proposed mandatory cross-licensing of drug patents, price limits, and restrictions on marketing in an effort to lower drug prices, the final legislation was oriented solely to drug safety and efficacy standards. Subsequent to passage of the Kefauver-Harris Amendments to the Food, Drug & Cosmetic Act in 1962, FDA promulgated guidelines detailing approved methods for clinical testing, enforced a strictly quantitative approach of evaluating drug applications, and began using its new authority to postpone or reject New Drug Applications.
Pharmaceutical firms responded to the thalidomide tragedy and subsequent regulations by investing greater resources in preclinical and clinical testing. Trials that previously were carried out on populations of tens or hundreds of patients soon grew to the thousands. Within a decade of enactment of the Kefauver-Harris Amendments in the U.S., however, even large companies with extensive research and testing programs began to complain of a decline in the number of new drugs approved for marketing. Drug companies then diversified into a range of other businesses including medical devices, diagnostics, optics, cosmetics, foodstuffs, and household goods. American firms increased sales overseas and also expanded international research with new labs in Europe, South America, and Asia.
The period between 1960 and 1980 also saw challenges to the authority of the medical profession in the form of feminist criticisms of patriarchy, publication of the influential book "Our Bodies, Ourselves" (1973) by the Boston Women's Health Book Collective, and expansion of disease-based organizations for childhood disorders and cancer. This was also the era when "the pill"--the birth-control pill--became a common term as pharmaceutically based birth control connected to significant social changes.



Join the conversation
Contact the reporter
Submit a Letter to the Editor for publication
Engage with us on Twitter