Advertisement
Grab your lab coat. Let's get started
Welcome!
Welcome!
Create an account below to get 6 C&EN articles per month, receive newsletters and more - all free.
It seems this is your first time logging in online. Please enter the following information to continue.
As an ACS member you automatically get access to this site. All we need is few more details to create your reading experience.
Not you? Sign in with a different account.
Not you? Sign in with a different account.
ERROR 1
ERROR 1
ERROR 2
ERROR 2
ERROR 2
ERROR 2
ERROR 2
Password and Confirm password must match.
If you have an ACS member number, please enter it here so we can link this account to your membership. (optional)
ERROR 2
ACS values your privacy. By submitting your information, you are gaining access to C&EN and subscribing to our weekly newsletter. We use the information you provide to make your reading experience better, and we will never sell your data to third party members.
Pharmaceuticals
Stents That Heal
Researchers modify artery-opening devices with peptide that triggers blood vessel repair
by Lauren K. Wolf
October 10, 2011
| A version of this story appeared in
Volume 89, Issue 41
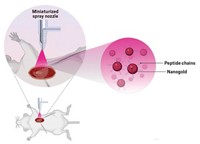
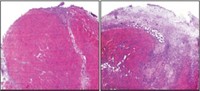
Not only can stents—the wire scaffolds that prop open blocked arteries—be functionalized with drugs to reduce inflammation caused by their insertion, but now they can also be modified with molecules that promote blood vessel healing. A research team led by Oliver Soehnlein and Christian Weber of Germany’s Ludwig Maximilians University, in Munich, showed that nickel-titanium alloy stents coated with an antimicrobial peptide from the cathelicidin family significantly increased the openings in clogged arteries of mice and improved the coverage of healthy cells in the vessels’ inner linings (Sci. Transl. Med., DOI: 10.1126/scitranslmed.3002531). When physicians implant stents into arteries, a small amount of damage occurs that triggers an immune response. In most cases, anti-inflammatory drugs bound to the inserted stents prevent reblocking of the vessels with scar tissue. But for about 10% of patients, according to Weber, arteries narrow again and blood clots sometimes form. The new strategy, which takes advantage of a cathelicidin peptide’s ability to recruit endothelial repair cells to an injured area, should further reduce that percentage, Weber adds. The next step for the team, he says, will be to develop and test a similar stent platform for humans.



Join the conversation
Contact the reporter
Submit a Letter to the Editor for publication
Engage with us on Twitter