Advertisement
Grab your lab coat. Let's get started
Welcome!
Welcome!
Create an account below to get 6 C&EN articles per month, receive newsletters and more - all free.
It seems this is your first time logging in online. Please enter the following information to continue.
As an ACS member you automatically get access to this site. All we need is few more details to create your reading experience.
Not you? Sign in with a different account.
Not you? Sign in with a different account.
ERROR 1
ERROR 1
ERROR 2
ERROR 2
ERROR 2
ERROR 2
ERROR 2
Password and Confirm password must match.
If you have an ACS member number, please enter it here so we can link this account to your membership. (optional)
ERROR 2
ACS values your privacy. By submitting your information, you are gaining access to C&EN and subscribing to our weekly newsletter. We use the information you provide to make your reading experience better, and we will never sell your data to third party members.
Biological Chemistry
Movers And Shakers
C&EN Talks With Alan Kozikowski
A medicinal chemist who is skeptical of the need for and effectiveness of psychiatric drugs
by Stu Borman
July 30, 2012
| A version of this story appeared in
Volume 90, Issue 31
Cheerleading pieces about drug discovery achievements often appear in scientific media, including in C&EN. Downsides to drug discovery and the unintended consequences of drugs don’t get as much attention. Alan P. Kozikowski is one researcher who has begun to acknowledge such difficult matters more openly as his career has matured. He offers some cautionary notes about psychiatric drugs, his area of specialization.
Kozikowski leads a drug discovery program in the department of medicinal chemistry and pharmacognosy at the University of Illinois, Chicago. He acknowledges the good that many drugs have achieved in alleviating suffering of some psychiatric patients. Nevertheless, he criticizes how some psychiatric drugs are developed, prescribed, and used.
Kozikowski earned a Ph.D. in organic chemistry at the University of California, Berkeley. He adopted neuroscience in a sabbatical at Georgetown University and has focused on neurochemistry and psychiatric drug discovery in academic positions at the University of Pittsburgh; the Mayo Clinic in Jacksonville, Fla.; Georgetown University Medical Center; and now at UIC. He also founded a company called Acenta Discovery, dedicated to the discovery of antidepressants. He has since sold the firm to PsychoGenics, a research services and testing provider.
Some neuropsychiatric drugs are administered irresponsibly, Kozikowski now believes. He was having doubts about the value of psychiatric drugs when he came across the 2001 book “Mad in America: Bad Science, Bad Medicine, and the Enduring Mistreatment of the Mentally Ill,” by journalist Robert Whitaker. The book was “a real eye-opener,” he says, and it has helped shape his current views. It makes a compelling case, he says, that many drugs for central nervous system (CNS) disorders do “more harm than good.”
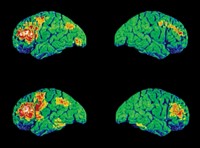
According to Kozikowski, he and others in the field of CNS drug discovery “may think we know what we are doing. We may think we are clever enough to invent a magic bullet for a brain disease by making a small molecule that interacts with a specific receptor, transporter, or enzyme. But we may in fact be fooling ourselves. There’s a level of impossibility in the idea that a single small molecule can fix a complex organ like the brain.”
Some psychiatric diagnoses, Kozikowski believes, have “rocky” foundations. “Some conditions are just part of life” and don’t require pharmaceutical intervention, he says. As an example he points to shift-work sleep disorder, the symptoms of which include insomnia and oversleepiness. Provigil (modafinil) is sometimes prescribed for the sleepiness caused by this condition. But Provigil’s official website concedes that the drug does not cure the disorder, does not alleviate all sleepiness, and does not take the place of enough sleep. In addition, modafinil has serious side effects that include severe dermatologic reactions. “So is this diagnosis and drug treatment really appropriate?” Kozikowski asks. “We already know that a person needs to have a good night’s sleep to function properly.”
Powerful psychotropic drugs like Provigil “have been developed for conditions that are nebulous at best and in the end cause far more harm than they are intended to fix,” he says. “My thinking, after many years of CNS research, is that we should take a very circumspect view of what conditions we think we can fix.”
Placebos “can work as well as approved drugs in double-blind placebo-controlled studies,” he notes. “Give a person a sugar pill for depression, let them think it is a possible palliative, and they may begin to think and feel better. The reverse is also true: Tell someone they have a problem, and they may begin to believe there is something wrong.”
In addition, too many psychiatric drugs are being prescribed to children, he says. Psychiatrists cannot agree even on the definition of attention deficit hyperactivity disorder (ADHD), he points out. “About 6 million kids in the U.S. are believed to be on medications for ADHD,” he says. “One of the most highly prescribed drugs for ADHD is Ritalin. Pharmacologically, Ritalin behaves pretty much like cocaine. It can be addictive and can cause anxiety, paranoia, insomnia, headaches, nausea, and chromosome aberrations. But psychiatrists may not warn parents about these side effects when they suggest their kids be given Ritalin.”
An ADHD diagnosis “may be an easy solution for a difficult kid who needs some quality time with parents or teachers,” he says. “While drug intervention may be required in certain acute cases of ADHD, likely we should not label so many adolescents with a neuropsychiatric condition that may simply resolve itself with time. Such a label marks them for life and can contribute to problems rather than solve them.”
Not only psychiatrists, “but also neuroscientists and chemists know far less about the brain than they may let on,” he adds. “But our activity moves forward relentlessly to the creation of medicines to fill the drug pipeline. Voltaire got it right: ‘Doctors are men who prescribe medicines of which they know little, to cure diseases of which they know less, in human beings of whom they know nothing.’ ”
Kozikowski believes a careful reexamination of the fields of CNS drug discovery and psychiatry is needed today. “Too many of us are working too hard to raise grant money for psychiatric drug discovery,” he says, “but we don’t think enough, or at all, about what future havoc we may be creating.”





Join the conversation
Contact the reporter
Submit a Letter to the Editor for publication
Engage with us on Twitter