Advertisement
Grab your lab coat. Let's get started
Welcome!
Welcome!
Create an account below to get 6 C&EN articles per month, receive newsletters and more - all free.
It seems this is your first time logging in online. Please enter the following information to continue.
As an ACS member you automatically get access to this site. All we need is few more details to create your reading experience.
Not you? Sign in with a different account.
Not you? Sign in with a different account.
ERROR 1
ERROR 1
ERROR 2
ERROR 2
ERROR 2
ERROR 2
ERROR 2
Password and Confirm password must match.
If you have an ACS member number, please enter it here so we can link this account to your membership. (optional)
ERROR 2
ACS values your privacy. By submitting your information, you are gaining access to C&EN and subscribing to our weekly newsletter. We use the information you provide to make your reading experience better, and we will never sell your data to third party members.
Neuroscience
Limits Of Lithium
It helps millions with bipolar disorder, but toxicity problems and side effects have scientists looking for alternatives by analyzing the drug’s mysterious mechanism
by Bethany Halford
March 25, 2013
| A version of this story appeared in
Volume 91, Issue 12

When something goes wrong with the inner workings of the body, we call it a disease. When things go awry in the mind’s fine machinery, we call it madness. Risdon Slate knows all about that. It has been more than 25 years since the events that led to his diagnosis of bipolar disorder. But he has no trouble recalling them.
In 1986, he was a 26-year-old U.S. probation officer visiting Miami for training. At one point, he remembers sitting in his hotel bar and getting into an argument with a man whom he perceived was playing the role of his father. “I actually believed that I was on the set of ‘Miami Vice’ and that I was going to be in an episode of the TV show,” Slate says. The police got involved, and Slate told officers that he would not answer any questions unless they were posed to him by Sonny Crockett, the fictional undercover police officer and central character of “Miami Vice.”
The retelling is almost comical, but the consequences for Slate were anything but. As a result of his bipolar disorder, Slate lost his job as a U.S. probation officer. His wife left him. A few years later, after a doctor took him off medication, Slate experienced a second manic episode, which led to an arrest (which has since been expunged) and a brutal physical assault while he was in jail. A bipolar patient swings between bouts of mania—when a patient can feel irrationally euphoric—and depression.
For a PDF of this article, visit http://cenm.ag/biopolar.
For the past 20 years though, Slate has managed to keep his disorder in check thanks to the drug lithium. “Taking the medication has been the key,” says Slate, now a professor of criminology at Florida Southern College. “It is essentially saving my life.”
Like Slate, 9 million people in the U.S. struggle with the disease at some point in their lives, according to the National Institute of Mental Health. Although roughly a dozen drugs are approved to treat bipolar mania and prevent or delay the onset of manic or depressive episodes, in many ways, lithium stands alone. Psychiatrists often turn to lithium—usually given as the salt lithium carbonate—as a first-line drug for patients. Its ability to calm the highs of mania and lift the lows of depression has been known for more than 60 years. It’s the only medication that demonstrably reduces the risk of suicide in bipolar patients. And it’s inexpensive.
But lithium is not a panacea. The drug’s therapeutic window is very narrow—that is, its toxic dose is only about two to three times higher than its therapeutic dose. Patients who take lithium also need to have the ion monitored in their blood to make sure it’s below toxic levels. And there are the side effects: tremors, frequent urination, thyroid problems, weight gain, and, in some cases, kidney failure.
In the hope of skirting lithium’s limitations, scientists are trying to figure out exactly how the drug works and, in particular, hunt down its targets. The idea is this: Because lithium is an ion, it hits several different cellular targets, which is why it has so many side effects. If scientists can figure out which of those targets are responsible for its mood-stabilizing properties, they might be able to hit them specifically, using a small molecule that doesn’t have lithium’s downsides.
“For some percentage of patients, lithium really does have a lot of the characteristics of an ideal treatment,” says psychiatrist Gary S. Sachs, founding director of the Bipolar Clinic & Research Program at Massachusetts General Hospital. “However, that is a relatively small percentage of patients.”
Other drugs approved to treat bipolar disorder were originally developed as anticonvulsants to treat epilepsy or as antipsychotics to treat schizophrenia. Thanks to their ability to level out certain moods, the drugs have been used to treat bipolar patients. It’s not clear how these drugs work either, and they often have more adverse side effects than lithium. All bipolar medications carry the U.S. Food & Drug Administration’s “black box” warning, Sachs points out, indicating they carry the risk of death. “Patients aren’t in a hurry to take those drugs,” he says.
“People find the side effects aversive, so they find ways to go off their medicine,” adds psychiatrist Kenneth Duckworth, medical director of the National Alliance on Mental Illness.
Scientists don’t really know what causes bipolar disorder, which was once known as manic depressive illness. It can strike at any age.
The disorder is unique among psychiatric illnesses, Duckworth points out, because people experience one phase of it, hypomania, positively. “People feel funnier, sexier, and more energetic,” he explains. They don’t want to take their medication, but they may be on their way to mania and psychosis.
Doctors split bipolar patients into two subgroups. Those with bipolar disorder type I, like Slate, have had at least one full-blown manic episode. Patients with bipolar disorder type II experience hypomania but not mania. Both type I and type II patients wrestle with depression, usually for far longer periods than they experience hypomania or mania.
“My depression feels like hell,” says Rebecca Gatlin, a 30-year-old nursing student who was diagnosed with bipolar disorder at age 19. “You have to push yourself to do every little thing,” Gatlin says. “You put so much effort into getting out of bed and brushing your teeth. Everything takes so much effort that you’re so exhausted and you walk around listless. You’re so exhausted from the littlest thing.
“You know that there are only two ways to get through it—to hang on until it lets up and things get better or the medicine kicks in, or you make a plan to end your life, and that’s not really a viable option,” Gatlin says. “You’re stuck holding on for life.”
“When you call depression mild, it’s sort of like saying you’ve had a mild heart attack,” Sachs says. The depressive phase of bipolar disorder can be extremely disabling, he says, and doctors don’t have many pharmaceutical options for treatment.
In 2007, Sachs and coworkers released the results of the Systematic Treatment Enhancement Program for Bipolar Disorder, or STEP-BD, the largest federally funded treatment trial ever conducted for bipolar disorder. They learned that antidepressants are no better at treating bipolar disorder than a placebo.
“So far, the track record of the so-called standard antidepressants has been terrible in terms of their ability to treat bipolar depression,” Sachs says. “None of them have proven to be effective, even though they are the most commonly prescribed drugs. So there is an area of great need to find novel compounds that would either treat or prevent depression in bipolar people.”
Lithium has a reputation for being moderately effective at treating or preventing bipolar depression. Scientists know that lithium displaces magnesium ions and inhibits at least 10 cellular targets. They have been able to narrow that range on the basis of what lithium inhibits at therapeutically relevant concentrations, roughly 0.6 to 1 mM.
One putative lithium target researchers have been pursuing for decades is inositol monophosphatase, or IMPase. The enzyme is part of the phosphatidylinositol signaling pathway. It strips the phosphate off of inositol phosphate to produce inositol, a key substance in the biosynthesis of compounds that trigger cellular responses.
There is some evidence that in bipolar patients the phosphatidylinositol signaling pathway becomes hyperactive. Inhibiting IMPase halts the pathway and depletes inositol. Adding credence to this theory, researchers have fingered inositol depletion in the mechanisms of two other bipolar medications—carbamazepine (Tegretol) and divalproex (Depakote), also called valproic acid.
“How can we really be sure that lithium works to treat bipolar disorder by inhibiting IMPase?” asks John R. Atack, director of translational drug discovery at England’s University of Sussex. “You make a good inhibitor of IMPase and see if it works in treating people with bipolar disorder.”
In the 1990s, Atack was part of a team at Merck & Co. trying to do just that. Reckoning they couldn’t do any medicinal chemistry on an elemental ion, because they couldn’t adjust its structure, Atack and coworkers developed IMPase inhibitors based on the enzyme’s substrate—inositol monophosphate.
Eventually they came up with an antagonist capable of inhibiting the enzyme at nanomolar concentrations. Polar phosphonate groups proved to be crucial to the compound’s ability to bind in IMPase’s active site, but the phosphonates kept the molecule from being bioavailable. “To get enzyme inhibition you need polar molecules,” Atack explains, “but those polar molecules don’t stand a very good chance of getting into the brain at high levels.”
The group tried to circumvent the problem by turning the molecule into an ester prodrug that could cross the membrane of the cell. It didn’t help. “If you inject that compound into an animal, it just sits there in a greasy lump,” Atack says.
Finally, the team used X-ray crystallography to study IMPase’s active site. “It confirmed what we already knew. The active site is very polar and therefore you need polar molecules to bind in it,” he says. Furthermore, the enzyme has no convenient greasy pockets where something less polar might do the job. “At that point, we didn’t really know where to go next,” Atack says, and the project was shelved. Talking about his work with IMPase is “like talking about an old girlfriend,” he adds. “She took a big chunk of my life, and I still have affection for her.
“It’s an unanswered question whether IMPase would be a good therapeutic target or not,” Atack adds. “Merck put a heroic effort into this and got nothing out of it. Perhaps it is an attractive but intractable target.”
Since then, scientists have largely been silent about any efforts to come up with IMPase inhibitors. Late last year, however, a team led by Grant C. Churchill and Sridhar R. Vasudevan, of the University of Oxford, in England, reported that the compound ebselen can inhibit IMPase (Nat. Commun., DOI: 10.1038/ncomms2320).
Ebselen, an anti-inflammatory antioxidant, was originally developed by Daiichi Sankyo, in Japan, to treat patients who had suffered a stroke. But the compound was never marketed and has since come off patent. It’s also part of the National Institutes of Health Clinical Collection—several hundred small molecules that have, to some extent, gone through the gamut of human clinical trials and have been found to be safe, but never reached final FDA approval.
In addition to inhibiting IMPase in vitro, the Oxford researchers found ebselen has lithium-like effects in a mouse model of mania. The compound calms mice that have taken amphetamine. Subsequent administration of inositol reverses the behavior, Churchill says, which is a clue that ebselen affects inositol recycling.
Since the report came out, Churchill says, a few psychiatrists have started to apply for funds to study ebselen’s effects in bipolar patients. At Oxford, doctors are giving the compound to a small group of healthy adults to see how it affects inositol processing in the brain. Ebselen has gone from identification as a potential bipolar treatment to human trials in about two years, Churchill points out. “That is incredibly fast for any drug discovery effort.”
Some, however, are skeptical that IMPase is a viable target for making lithium mimics. The target was discredited years ago, says Edward M. Scolnick, who served as president of Merck & Co. from 1982 through 2002. Rather, he believes the key to finding better treatments for bipolar disorder lies in unraveling the disease’s genetics. Currently chief scientist at Broad Institute’s Stanley Center for Psychiatric Research, Scolnick is part of an effort trying to do just that.
“The single largest risk factor for a person becoming bipolar is genetic,” Scolnick explains. Scientists can’t study the biochemistry of the living human brain, he points out, and imaging methods lack the sensitivity to pick up molecular causes. So, Scolnick says, the only way to get a handle of the underlying pathophysiology and biochemistry of bipolar disorder is to find the genes related to illness and see what biochemical pathways they point to. “Unless one understands the underlying biochemistry of the human disease—not some animal model that has no clear relationship to the human disease—one will never be able to make important new therapeutics,” he says.
Advertisement
Scolnick is not the only one to voice concerns about animal models for bipolar disorder. Psychiatrist Carlos A. Zarate, chief of the National Institute of Mental Health’s (NIMH) Section on the Neurobiology & Treatment of Mood Disorders, also notes that these models of the disease leave something to be desired.
Typically, the complex mental state of mania is modeled by giving mice amphetamines. Scientists test antidepressants on animals by forcing rodents to swim or suspending them by their tails. The length of time the creature swims or struggles is supposed to be indicative of the antidepressant’s efficacy.
Correlating animal tests that take only a few minutes with a patient who’s suffered from a disease for decades is problematic, Zarate says. With such imprecise animal models and uncertainty about a disease’s pathophysiology, he adds, it’s no wonder that companies are hesitant to get into psychiatric diseases.

Until the genetics become clear enough to show what pathways to pursue, Scolnick says, he and his colleagues at the Stanley Center are working on developing inhibitors of another putative therapeutic target of lithium: glycogen synthase kinase-3, or GSK-3.
GSK-3 appends phosphate groups to serine and threonine amino acid residues. It functions in many pathways and has been implicated in diseases such as Alzheimer’s, type 2 diabetes, and cancer. “What it does in the human brain is very hard to tell,” says Peter S. Klein, the University of Pennsylvania professor of medicine who discovered that lithium inhibits GSK-3. One possibility is that lithium’s inhibition of GSK-3 turns on the Wnt signaling pathway, which stimulates the generation of neurons.
Inhibitors of GSK-3 are currently in clinical trials to treat progressive supranuclear palsy and certain cancers. But there are few reports of GSK-3 inhibitors being developed for bipolar disorder.
In 2007, researchers led by Alan P. Kozikowski, a chemistry professor at the University of Illinois, Chicago, reported that 3-benzofuranyl-4-indolylmaleimides are potent and selective inhibitors of GSK-3 (J. Am. Chem. Soc., DOI:10.1021/ja068969w). The most promising of the compounds Kozikowski’s team made calmed hyperactive behavior in mice that took amphetamine—the same model system of mania the ebselen researchers used. But Kozikowski says funding for the project dried up and his group hasn’t worked on GSK-3 inhibitors for years.
Scolnick says his group at the Stanley Center has come up with some selective GSK-3 inhibitors, but he declined to comment on their structures. Now, he says, they’re doing classical medicinal chemistry to boost the molecules’ pharmaceutical profiles.
Some people are concerned about using GSK-3 inhibitors, Klein says. Inhibiting GSK-3 potently activates the Wnt pathway, he says, and activation of the Wnt pathway is a key step in roughly 90% of colorectal carcinoma. “The worry is that you’re going to cause cancer,” he says. “In the many years that lithium has been studied, there has been no increased incidence of leukemia or cancers in people taking lithium,” Klein is quick to add, “but a more potent GSK-3 inhibitor could be oncogenic.”
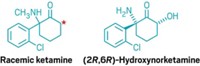
One drug that’s recently grabbed the spotlight for treating bipolar depression is the anesthetic agent ketamine (C&EN, Aug. 23, 2010, page 8). In the past few years, trials in people have shown that a subanesthetic infusion of the drug can relieve the symptoms of depression and suicidal urges in a matter of hours, says NIMH’s Zarate, who conducted some of the studies. The effect lasts about a week, whereas commonly prescribed antidepressants usually take weeks to work.
Ketamine is a derivative of phencyclidine, or PCP, and acts as an antagonist of N-methyl-
“It’s really ignited interest in drug discovery and development,” Zarate says. His group and others are looking into compounds that act like ketamine but last longer and don’t have ketamine’s psychotropic side effects.
Although interest may be picking up, efforts from the pharmaceutical industry to develop new drugs specifically to treat bipolar disorder remain rare. Last year PhRMA, the Pharmaceutical Research & Manufacturers of America, put out a report on medicines in clinical trials to treat mental illness. Most of the 12 compounds listed for bipolar disorder fall into the category of anticonvulsant or antipsychotic. Even the few that don’t fit into those categories were originally developed for other uses.
New drugs come at a price, though. “The expense of our medication is a problem,” says Leah Nakamura, who has bipolar disorder type I and coordinates several support groups for people with the illness. She points out that having bipolar disorder can make it tough to keep a job, so people lose their health insurance and can’t afford their medication.
Although lithium costs less than a dollar a day, drugs still under patent protection, such as aripiprazole (Abilify), can cost hundreds of dollars each month. “At some point you just can’t afford it,” Nakamura says, “and these are lifesaving drugs.”
Nakamura wishes she had better medications to choose from. She’s currently on her fifth drug to keep her bipolar symptoms at bay. If this one doesn’t work, she says, she doesn’t have many options, but she is still hopeful for the future. Nakamura says, “I tell our young adult support group, ‘Hang in there. Hope is on the way. They’re working on treatments for us.’ ”
- Limits Of Lithium
- Discoveries: How Lithium Became A Drug
For a PDF of this article, visit http://cenm.ag/biopolar.





Join the conversation
Contact the reporter
Submit a Letter to the Editor for publication
Engage with us on Twitter