Advertisement
Grab your lab coat. Let's get started
Welcome!
Welcome!
Create an account below to get 6 C&EN articles per month, receive newsletters and more - all free.
It seems this is your first time logging in online. Please enter the following information to continue.
As an ACS member you automatically get access to this site. All we need is few more details to create your reading experience.
Not you? Sign in with a different account.
Not you? Sign in with a different account.
ERROR 1
ERROR 1
ERROR 2
ERROR 2
ERROR 2
ERROR 2
ERROR 2
Password and Confirm password must match.
If you have an ACS member number, please enter it here so we can link this account to your membership. (optional)
ERROR 2
ACS values your privacy. By submitting your information, you are gaining access to C&EN and subscribing to our weekly newsletter. We use the information you provide to make your reading experience better, and we will never sell your data to third party members.
Biological Chemistry
For Drug Overdoses, These Nanomaterials Could Be The Antidote
Chemists work to develop ways to pull a broad range of poisons from overdose patients
by Bethany Halford
November 16, 2015
| A version of this story appeared in
Volume 93, Issue 45

Poisoning from drug overdoses has become a growing problem in the U.S. More than a million people are treated in U.S. hospital emergency rooms each year for unintentional poisonings, most of which are caused by illicit or prescription drugs. Although most of these patients require relatively simple care, more severe cases can be tough to treat.

In 2013, the most recent year for which data are available, 38,851 people in the U.S. died from unintentional poisonings, according to the National Center for Health Statistics. And the death rate from poisoning has more than doubled since 2000, the center notes. In fact, poisoning accounted for more injury-related deaths than either motor vehicle accidents or firearm fatalities.
For certain drug-related poisonings, there are readily available antidotes: naloxone for opioids and N-acetylcysteine for acetaminophen. But for most drugs, there are no antidotes, and often patients don’t know or can’t tell doctors what drug they’ve overdosed on. Doctors resort to stomach pumping and the use of activated charcoal if they can treat a patient quickly, or in more advanced cases of poisoning, they must rely on dialysis and blood filtration.
Seeking a better way of pulling poisons from patients, chemists have been working to develop wide-spectrum antidotes. They envision that such generic treatments would neutralize a toxic compound or help the body to eliminate it, regardless of its chemical composition.
About 10 years ago, Jean-Christophe Leroux, a chemistry professor at the Swiss Federal Institute of Technology (ETH), Zurich, who specializes in drug delivery, started developing such a treatment by looking at his research in reverse. “We realized there were not very many systems to treat drug intoxication,” he says. “So we asked ourselves: Can we use our knowledge in drug delivery and nanotechnology to develop more efficient systems for detoxification?”
Leroux’s team got inspiration from a 2006 case in which doctors injected an intravenous lipid emulsion to resuscitate a patient who was overdosing on the local anesthetic bupivacaine. Such emulsions are usually used to deliver nutritional supplements, but work in animals had shown that they could also sequester bupivacaine and other drugs, so the doctors decided to give it a try. “The lipids attract some of the drug back into the bloodstream and reduce the effect of the drug,” Leroux explains. “It seems to work. It’s just not very efficient.”
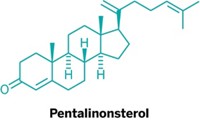
Leroux wondered if liposomes—particles that are used for drug delivery—would work better. Liposomes are hollow spheres made from lipid bilayers: Lipid molecules arrange themselves so that their polar head groups line the outside and inside of the sphere, sandwiching their hydrophobic tails in between. Either basic or acidic buffers fill the liposome’s core so that a neutral drug might diffuse through the greasy bilayer into the liposome, become ionized, and then be trapped.
This method is often used to load liposomes with drugs for delivery, Leroux says, but he thought it might also be used to pull drugs from the bloodstream. Many drugs, he explains, are weak bases and liposomes loaded with acidic buffer could protonate them, sequestering them within the liposome.
Leroux’s group has used such liposomes to effectively reverse overdoses of the antidepressant amitriptyline and calcium channel blockers diltiazem and verapamil in animal models. Animals treated with liposomes recovered more quickly than those treated with lipid emulsions.
“The good thing about liposomes is that there are a lot of parameters that you can play with,” says University of Florida chemical engineering professor Anuj Chauhan. For example, his group has explored liposomes made with lipids that have charged head groups. These groups attract drugs that are ionized at physiological pH, such as antidepressants. The ionized portion of the drug associates with the charged head groups, and the drug’s hydrophobic region slips between the oily tail groups. This dual interaction, Chauhan explains, makes the liposome particularly effective as a drug trap.
Chauhan has used this approach to treat overdoses of the antidepressant clomipramine in rabbits. He points out that the liposomes eventually break down, releasing the drug back into the bloodstream. But they release the drug more slowly, so the body isn’t overwhelmed.
To try to remove drugs entirely from the body, Leroux’s team has adapted an existing technique in which doctors flush a fluid into the peritoneal cavity—the space around the belly—and then remove it once it has absorbed certain molecules. In the new version, the researchers use microscale liposomes to eliminate several different drugs, including propranolol, haloperidol, and phenobarbital in animal studies. Leroux has even cofounded a company, Versantis, to commercialize the technology.
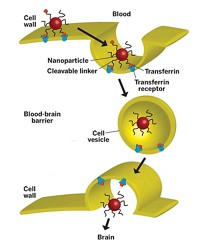
These technologies illustrate “a great connection between these two problems of drug delivery and drug detoxification,” says Liangfang Zhang, a nanoengineering professor at the University of California, San Diego. Zhang notes that the same features that make nanoparticles good drug delivery agents, such as their ability to travel to all parts of the body while evading an immune response, also make them good materials for sequestering drugs from the body. “As the poison molecules spread out in the bloodstream, you need to find them, absorb them, and then divert them away from their original cellular target,” Zhang explains.
Instead of developing treatments for drug poisonings, Zhang’s group has been working on a type of nanoparticle “sponge” that soaks up any toxin that targets red blood cells, such as protein toxins from bacteria or snake venom. The particles are about 100 nm across. They have polymer cores that are coated with a red blood cell membrane and basically serve as decoys circulating in the blood, Zhang says. When toxic chemical or biological molecules that target red blood cells encounter the nanosponge, they cannot distinguish between it and a genuine red blood cell, so they attack the sponge and get caught.
“In a conventional detoxification approach, we need to know what the toxin is, and we try to design small-molecule inhibitors or an antibody to neutralize it,” Zhang says. “We tried to look at this from a different angle. We looked at the working mechanism of all these different types of toxins. No matter what their molecular structure is, they do the same job: They target host cells.”
Zhang’s group has used their nanosponges in mice to trap α-toxin, a pore-forming toxin that’s a key component in Staphylococcus aureus infections. They’ve also used it to treat poisoning from organophosphates—toxic compounds found in insecticides and nerve gas—and they’ve demonstrated that the same nanoparticles can clear antibodies associated with autoimmune disorders. Zhang is currently working on an Investigational New Drug Application for the nanosponges.
It will take years for these types of general antidotes to be ready for doctors to use, ETH Zurich’s Leroux notes. Because it’s hard to set up a clinical trial for poisoning, he suspects the liposomes and nanoparticles will first be used in trials for nonpoisoning ailments, such as a metabolic disorder that causes an excess of ammonia in the blood. Then when the liposomes and nanoparticles have been determined to be safe, doctors will use them off-label to treat poisoning, just as they now do with lipid emulsions.



Join the conversation
Contact the reporter
Submit a Letter to the Editor for publication
Engage with us on Twitter