Advertisement
Grab your lab coat. Let's get started
Welcome!
Welcome!
Create an account below to get 6 C&EN articles per month, receive newsletters and more - all free.
It seems this is your first time logging in online. Please enter the following information to continue.
As an ACS member you automatically get access to this site. All we need is few more details to create your reading experience.
Not you? Sign in with a different account.
Not you? Sign in with a different account.
ERROR 1
ERROR 1
ERROR 2
ERROR 2
ERROR 2
ERROR 2
ERROR 2
Password and Confirm password must match.
If you have an ACS member number, please enter it here so we can link this account to your membership. (optional)
ERROR 2
ACS values your privacy. By submitting your information, you are gaining access to C&EN and subscribing to our weekly newsletter. We use the information you provide to make your reading experience better, and we will never sell your data to third party members.
Materials
New Layered Design Could Lead To Better Implantable Glucose Sensors
Biosensors: A stack of gels and polymers yields a sensitive, selective glucose detector
by Prachi Patel
February 2, 2015

Diabetic patients track their glucose levels by regularly pricking their fingertips to get blood samples. An implantable glucose sensor would be more convenient. It could be left in for long periods of time and could allow for continuous monitoring. Toward that goal, researchers report a novel sensor consisting of a stack of different gel and polymer films that can detect small concentration changes in glucose in real time (Langmuir 2015, DOI: 10.1021/la504358t).
Today’s glucose meters use disposable polymer test strips embedded with the enzyme glucose oxidase. Glucose reacts with the enzyme to produce hydrogen peroxide, which oxidizes at an electrode to create an electrical signal.
To replace the disposable strips, scientists have made continual-use sensors with sol-gels, which are highly porous networks of silane monomers that can hold a large amount of enzyme in a small volume. But gel-based sensors made so far are either unstable, not sensitive enough, or have a small detection range; normal blood glucose concentrations can range from 3 to greater than 20 mM. Another downside is that these sensors also respond to other chemicals that can be present in the bloodstream, such as acetaminophen and ascorbic acid.
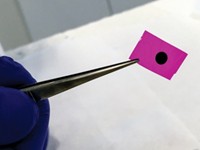
Michael C. Leopold, a chemist at the University of Richmond, in Virginia, and his colleagues addressed those issues with a novel layered design. They deposited a mix of silane monomers containing glucose oxidase on a platinum electrode and then added a layer of enzyme-free silane monomers on top. They allowed these two layers to age to form xerogels—a kind of high-density aerogel—and then capped them with a polyphenol layer and a polyurethane layer. The various layers formed a stacked film several hundred micrometers thick.
The two polymer layers serve as a size-selective filter, letting glucose through but keeping other compounds out. The enzyme-free xerogel layer slows down glucose molecules as they flow into the enzyme-loaded gel. This is important for continuous use because it allows the enzymes to reset before the next wave of glucose molecules reaches them, Leopold says.
The layered sensors could detect spikes and drops in glucose concentrations ranging from 8 to 20 µM in 15 to 25 seconds. All of them worked at glucose concentrations up to 28 mM. The sensors performed well for two weeks and did not respond to other compounds such as acetaminophen.
Leopold envisions that a biosensor consisting of ultrathin wires or intravenous needles coated with the sensor stack could be implanted under the skin for continuous monitoring.
Francis P. Zamborini, a chemist at the University of Louisville, in Kentucky, says that the sensor is impressive because it combines high sensitivity, a wide detection range, high selectivity, and good stability. “Many other glucose sensors show some of these desirable qualities, but not all,” he says. Because they work for about two weeks, “these sensors could find use in short-term medical settings, such as emergency rooms, intensive care units, or maternity wards.”




Join the conversation
Contact the reporter
Submit a Letter to the Editor for publication
Engage with us on Twitter