Advertisement
Grab your lab coat. Let's get started
Welcome!
Welcome!
Create an account below to get 6 C&EN articles per month, receive newsletters and more - all free.
It seems this is your first time logging in online. Please enter the following information to continue.
As an ACS member you automatically get access to this site. All we need is few more details to create your reading experience.
Not you? Sign in with a different account.
Not you? Sign in with a different account.
ERROR 1
ERROR 1
ERROR 2
ERROR 2
ERROR 2
ERROR 2
ERROR 2
Password and Confirm password must match.
If you have an ACS member number, please enter it here so we can link this account to your membership. (optional)
ERROR 2
ACS values your privacy. By submitting your information, you are gaining access to C&EN and subscribing to our weekly newsletter. We use the information you provide to make your reading experience better, and we will never sell your data to third party members.
Biological Chemistry
Nanoparticles Hit Cancer’s Moving Target
Nanomedicine: A nanoparticle that targets two metastatic markers can find cancer cells as they spread from a primary tumor site
by Katherine Bourzac
August 26, 2015

Though most cancer therapies treat tumors as monoliths, the cells evolve and change their behavior over time. For example, they can alter their gene expression pattern to escape from the primary tumor and spread throughout the body. Now, researchers have developed a nanoparticle that targets cancer cells at two different stages of metastasis, which could make it possible to prevent the disease from spreading (ACS Nano 2015, DOI: 10.1021/acsnano.5b01552).
About 90% of cancer deaths are caused not by the initial tumor but by secondary tumors, or metastases, that often take root in the lungs, bone, liver, or brain. These metastatic cells commonly survive chemotherapy and are “buried in the large population of healthy cells in the body,” says Efstathios Karathanasis, a biomedical engineer at Case Western Reserve University. “To kill them all, the concentration of the drug would have to be so high that you would kill the patient.”
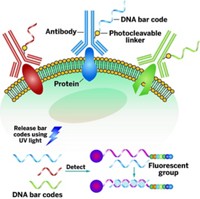
By packaging small molecule drugs inside nanoparticles, a number of researchers hope to develop therapies that will deliver a highly concentrated dose of a drug only to tumor cells, while sparing healthy tissue. They do this by decorating the drug-carrying nanoparticles with a ligand targeted to a marker found only on cancer cells.
Karathanasis wanted to refine this active targeting approach even further. Cancer biology, he says, suggests that targeting one cancer marker is not enough. No single characteristic protein receptor is overexpressed on all the cancer cells from the same tumor, in the same patient, at a given time. So he decided to target two protein markers that are characteristic of the different stages tumor cells undergo during the early stages of metastasis.
To test this idea, his team decorated a 100-nm-diameter liposome with ligands that target two surface proteins expressed on metastatic cancer cells after they have escaped from a tumor and are circulating in the bloodstream. Both proteins help circulating tumor cells exit the bloodstream at a new site so that they can establish a new tumor. One protein, selectin, helps cancer cells circulating in the blood start to roll along the inside surface of a blood vessel. The second protein, integrin, helps these rolling cells firmly attach to the blood vessel before exiting and seeding a new tumor.
To see whether the nanoparticle could actually find rogue cancer cells, Karathanasis’s group tested it in two different mouse models of metastatic triple-negative breast cancer, an extremely aggressive form of the disease. They injected fluorescently or radioactively labeled nanoparticles into the mice and saw that the nanoparticles hit the mark. They caught about 90% of the micrometastatic sites—small clusters of cancer cells 10 to 30 μm in size, Karathanasis says.
Because integrins and selectins are also markers of inflammation and cardiovascular disease, the researchers will need to test the nanoparticles for side effects, Karathanasis says. They also plan to test this recognition system with a nanoparticle that’s carrying a cancer drug.
Ravi V. Bellamkonda, chair of biomedical engineering at Georgia Tech and Emory University, is impressed with the dual targeting strategy. “It recognizes that tumors are not monolithic and that, within each tumor or within each patient, one might have tumors at different stages of development or metastatic spread,” he says. That brings nanotherapy design into better alignment with the current understanding of cancer biology.




Join the conversation
Contact the reporter
Submit a Letter to the Editor for publication
Engage with us on Twitter