Advertisement
Grab your lab coat. Let's get started
Welcome!
Welcome!
Create an account below to get 6 C&EN articles per month, receive newsletters and more - all free.
It seems this is your first time logging in online. Please enter the following information to continue.
As an ACS member you automatically get access to this site. All we need is few more details to create your reading experience.
Not you? Sign in with a different account.
Not you? Sign in with a different account.
ERROR 1
ERROR 1
ERROR 2
ERROR 2
ERROR 2
ERROR 2
ERROR 2
Password and Confirm password must match.
If you have an ACS member number, please enter it here so we can link this account to your membership. (optional)
ERROR 2
ACS values your privacy. By submitting your information, you are gaining access to C&EN and subscribing to our weekly newsletter. We use the information you provide to make your reading experience better, and we will never sell your data to third party members.
Biological Chemistry
A new dipstick test can rapidly distinguish between Zika and dengue fever infections
An international team has developed a way to easily differentiate the closely related viral infections
by Emma Hiolski
October 5, 2017
| A version of this story appeared in
Volume 95, Issue 40

The mosquito-borne viruses, Zika and dengue fever, plague developing countries around the world. Dengue can cause hemorrhagic fever, and Zika can lead to devastating congenital neurological defects. Properly diagnosing a patient with one of these infections is challenging, however, because the viruses are closely related.
Flavivirus nonstructural 1 (NS1) protein, the viral protein commonly targeted by antibody-based diagnostic tests, has approximately 70% sequence similarity between Zika and dengue viruses, says Kimberly Hamad-Schifferli, an engineer at University of Massachusetts, Boston. “It’s very hard to make antibodies that can distinguish between them.”
To tackle this problem, Hamad-Schifferli and Lee Gehrke, an immunobiologist at MIT and Harvard University, led a 53-person international team to develop a simple dipstick test that uses pairs of antibodies to sandwich NS1, allowing the scientists to distinguish between the two viruses (Sci. Transl. Med. 2017, DOI: 10.1126/scitranslmed.aan1589).
The team generated hundreds of antibodies against the NS1 protein using animal and cell models and then tested hundreds of antibody pairs to determine which combinations would be most sensitive and specific to the dengue and Zika viral proteins. The top pairs were used in the dipstick tests.
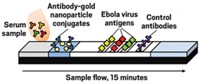
In the assay, gold nanoparticles tagged with one antibody bind to viral proteins in patient serum. The dipstick, coated with a second virus-specific antibody, wicks up the serum. In roughly 15 minutes, the virus protein is “sandwiched” between the two antibodies and the tagged gold nanoparticles accumulate on a test area on the dipstick, creating a red spot. The team confirmed the accuracy of these tests using serum samples from dengue and Zika patients from North and South America and India.
“This is an excellent piece of work,” comments Shamala Devi Sekaran, an immunologist at the University of Malaysia. “It certainly is very impressive, and they managed to evaluate a number of samples from different geographical areas, albeit not all.”
In addition to expanding the pool of clinical Zika and dengue samples, the team hopes to use the new method to develop rapid tests for other mosquito-borne diseases.


Join the conversation
Contact the reporter
Submit a Letter to the Editor for publication
Engage with us on Twitter