Advertisement
Grab your lab coat. Let's get started
Welcome!
Welcome!
Create an account below to get 6 C&EN articles per month, receive newsletters and more - all free.
It seems this is your first time logging in online. Please enter the following information to continue.
As an ACS member you automatically get access to this site. All we need is few more details to create your reading experience.
Not you? Sign in with a different account.
Not you? Sign in with a different account.
ERROR 1
ERROR 1
ERROR 2
ERROR 2
ERROR 2
ERROR 2
ERROR 2
Password and Confirm password must match.
If you have an ACS member number, please enter it here so we can link this account to your membership. (optional)
ERROR 2
ACS values your privacy. By submitting your information, you are gaining access to C&EN and subscribing to our weekly newsletter. We use the information you provide to make your reading experience better, and we will never sell your data to third party members.
Biological Chemistry
High-salt diet throws microbiome out of whack
Study in mice suggests rebalancing gut microbes might one day treat conditions linked to sodium intake
by Katharine Sanderson, special to C&EN
November 20, 2017
| A version of this story appeared in
Volume 95, Issue 46
It’s no longer just your doctor telling you to cut back on the salty foods. Your gut might be trying to send you a signal too.
Gut bacteria in mice change significantly after the animals have eaten a high-salt diet, researchers have found (Nature 2017, DOI: 10.1038/nature24628). And feeding the animals microbes to replace those lost because of this diet can help ameliorate some negative health effects, a finding that could lead to future treatments for conditions caused by high salt intake, the scientists say.
At Germany’s Experimental & Clinical Research Center, jointly operated by the Max Delbrück Center for Molecular Medicine and Charité—Medical University of Berlin, Nicola Wilck and coworkers gave one group of mice a high-salt diet and another group normally salted meals.
Over the course of the three-week diet, the team sequenced ribosomal DNA in the animals’ feces and coupled the results with a machine-learning algorithm to identify the microbes residing in their guts. After just 14 days of evaluation, the researchers observed that the mice eating more salt played host to lower levels of the mouse-specific bacterium Lactobacillus murinus.
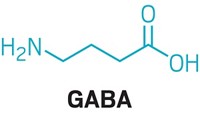
To test what role this microbe plays in mouse health, Wilck and his colleagues gave L. murinus to mice with high-salt-induced hypertension and to mice with a type of brain inflammation called actively induced experimental autoimmune encephalomyelitis (EAE). The real-world diseases mimicked by these lab-generated conditions have been linked to the malfunctioning of a certain type of immune cell, the TH17 cell. These cells also become more prevalent in animals and people who eat a lot of salt.
When given L. murinus, the mice with hypertension experienced reduced blood pressure, and those with EAE displayed less inflammation. The researchers also found that the number of TH17 cells decreased when these mice were given the replacement bacteria.
Encouraged by these results, the team ran a small-scale, limited-scope trial in humans. Twelve healthy men ingested 6 g of salt (NaCl) each day for 14 days. Similar to the mice, levels of various Lactobacillus microbes in their guts declined.
“The mouse microbiome varies on a daily basis, but compared with human beings, it is a fairly simple system,” Wilck says. For example, not every adult human has Lactobacillus in his or her microbiome. So he urges caution when specifically considering administering this type of bacteria as a probiotic treatment in humans.
David Relman at Stanford University agrees that these results won’t necessarily translate to humans. “The salt dose used in these mice was far beyond that which would be relevant to or tolerated by humans,” Relman says. But he notes that the results should prompt others to investigate with deliberate, well-controlled studies in humans. “If it can be shown that components of the human microbiota play a meaningful role in mediating the effect of dietary salt in promoting hypertension in some humans, this would be big,” Relman adds.





Join the conversation
Contact the reporter
Submit a Letter to the Editor for publication
Engage with us on Twitter