Advertisement
Grab your lab coat. Let's get started
Welcome!
Welcome!
Create an account below to get 6 C&EN articles per month, receive newsletters and more - all free.
It seems this is your first time logging in online. Please enter the following information to continue.
As an ACS member you automatically get access to this site. All we need is few more details to create your reading experience.
Not you? Sign in with a different account.
Not you? Sign in with a different account.
ERROR 1
ERROR 1
ERROR 2
ERROR 2
ERROR 2
ERROR 2
ERROR 2
Password and Confirm password must match.
If you have an ACS member number, please enter it here so we can link this account to your membership. (optional)
ERROR 2
ACS values your privacy. By submitting your information, you are gaining access to C&EN and subscribing to our weekly newsletter. We use the information you provide to make your reading experience better, and we will never sell your data to third party members.
Cancer
Some anticancer molecules are off target
Experiments in cell lines suggest that the molecules kill cancer cells through targets they weren’t designed to hit
by Leigh Krietsch Boerner
September 16, 2019

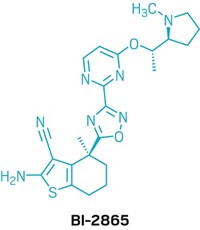
About 97% of small molecules that enter clinical trials for cancer don’t end up getting approved. Scientists want to better understand the factors that lead to so many failures. Now Jason Sheltzer, a cancer biologist at Cold Spring Harbor Laboratory, and coworkers may have found one. Through cell culture experiments, they determined that 10 clinical or preclinical molecules don’t kill cancer cells through the targets they were designed to hit, suggesting that the targets had been mischaracterized (Sci. Transl. Med. 2019, DOI: 10.1126/scitranslmed.aaw8412).
Scientists typically use a method called RNA interference (RNAi) to identify the targets of anticancer molecules. In this method, scientists apply synthetic RNAs to cancer cells in culture to try to trick the cells into not expressing a certain gene. If the gene codes for the protein target of a given anticancer molecule, that molecule will no longer be potent against the RNAi-treated cells, and the cells will survive.
But RNAi isn’t perfectly specific, Sheltzer says. “Oftentimes you won’t just block the expression of the gene you want,but a lot of different genes as well.” As a result, he says, scientists can’t be totally sure what protein their molecule targets. “The off-target effects may have been more significant than scientists previously realized, leading to a lot of false positives,” Sheltzer says.
To try to get more certainty, he and his team decided to use the gene-editing technique CRISPR to validate some targets. CRISPR is more exact than RNAi. The method cuts DNA at specific spots, which shuts down the gene sitting at the cut site. The team used CRISPR to snip the genes for the protein targets of 10 different anticancer molecules, 7 of which are currently or have been in clinical trials and 3 that are in preclinical development. They made these cuts in several different cancer cell lines and then tested the molecules on the cells.
The team was surprised to find that when they eliminated the proteins from the cancer cells, the cells still grew, suggesting that the targets weren’t essential for cancer cell survival and growth. Also, the molecules still killed the cancer cells even after expression of the target protein had been knocked down. “If you have a drug that’s specific for a particular protein, and then you get rid of that protein, then theoretically the drug should have no effect on the cancer cells,” Sheltzer says. These results suggested that the molecules must be killing the cancer cells through other unknown, off-target mechanisms, he says.
For one molecule, OTS964, the group pinpointed a possible correct target: the protein CDK11. When they mutated the CDK11 gene in a number of different cancer lines and treated the cells with lethal amounts of the molecules, the cells survived.
Sheltzer stresses that their findings are just in cell lines, which are different from tumors growing in actual people. He also says that their findings may not be relevant for rare types of tumors as his team tested only 32 different cancer cell lines.
But the findings suggest that knowing how a molecule kills cancer cells is paramount to creating a successful anticancer molecule, Sheltzer said at a press conference last week. If a molecule doesn’t work through the expected target and instead kills tumors through off-target mechanisms, there’s an increased chance that those other pathways are not relevant or behave differently when you move from cell lines in a lab to a patient in a clinic. And that can lead to failure in the clinic.
“For the small-molecule cancer drug development world, those who are not currently holding themselves to the standards represented in this paper, this work should be a wake up call,” says John Maxwell, a medicinal chemist at Tango Therapeutics.
Medicinal chemists always worry that there’s something else going on in cancer cells that complicates our understanding of how a given molecule works, says Donna M. Huryn, a medicinal chemist at the University of Pittsburgh School of Pharmacy. “This paper reminds you that that’s the case. We still need to continue to be vigilant.”
This work shows how important it is to use multiple approaches to validate a drug target before spending hundreds of millions of dollars to develop a set of small molecules as drug candidates, says Matthew Hall, a translational scientist at the National Center for Advancing Translational Sciences.
“What Sheltzer showed us by working backwards from drug candidates to genes is that we’re still not good enough” to precisely pinpoint a molecule’s target, Hall says. “It’s a really beautifully put together cautionary tale.”




Join the conversation
Contact the reporter
Submit a Letter to the Editor for publication
Engage with us on Twitter