Advertisement
Grab your lab coat. Let's get started
Welcome!
Welcome!
Create an account below to get 6 C&EN articles per month, receive newsletters and more - all free.
It seems this is your first time logging in online. Please enter the following information to continue.
As an ACS member you automatically get access to this site. All we need is few more details to create your reading experience.
Not you? Sign in with a different account.
Not you? Sign in with a different account.
ERROR 1
ERROR 1
ERROR 2
ERROR 2
ERROR 2
ERROR 2
ERROR 2
Password and Confirm password must match.
If you have an ACS member number, please enter it here so we can link this account to your membership. (optional)
ERROR 2
ACS values your privacy. By submitting your information, you are gaining access to C&EN and subscribing to our weekly newsletter. We use the information you provide to make your reading experience better, and we will never sell your data to third party members.
Infectious disease
Covid-19
Finding what cells the coronavirus can enter could help explain why it spreads so well
Two studies pinpoint nasal cells and others that express the molecules the virus uses to get inside
by Alla Katsnelson, special to C&EN
April 30, 2020
| A version of this story appeared in
Volume 98, Issue 17

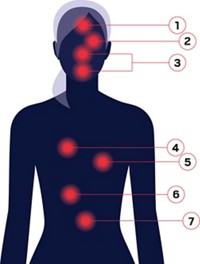
One of the many pressing mysteries that scientists are trying to solve about SARS-CoV-2, the novel coronavirus that causes COVID-19, is how it manages to spread so easily. Two recent studies provide some clues by pinning down cell types that express the two major proteins that the virus uses to sneak into cells—the cell surface receptor angiotensin-converting enzyme 2 (ACE2) and the enzyme transmembrane protease, serine 2 (TMPRSS2).
Both studies turned up two cell types in the nose—goblet cells and ciliated cells—that strongly express ACE2 (Nat Med. 2020, DOI: 10.1038/s41591-020-0868-6; Cell 2020, DOI: 10.1016/j.cell.2020.04.035). “These cells are located at the outermost layer of the nasal epithelium, making them highly accessible to the environment,” says Waradon Sungnak, an immunologist at the Wellcome Sanger Institute and first author of the Nature Medicine study. “This could allow them to be highly susceptible to infection and efficient in viral shedding,” he says, referring to the release of virus particles from infected cells.
Support nonprofit science journalism
C&EN has made this story and all of its coverage of the coronavirus epidemic freely available during the outbreak to keep the public informed. To support us:
Donate Join Subscribe
Although SARS-CoV-1, which caused the severe acute respiratory syndrome (SARS) epidemic of 2002–2003, also uses ACE2 to enter host cells, researchers had not previously identified nasal cells as viral targets. “That’s ultimately the most important ‘ah-ha’ in these papers,” says Michael Farzan, an immunologist and microbiologist at the Scripps Research in Flordia. Back in 2003, Farzan’s lab discovered ACE2 as the receptor SARS-CoV-1 exploits to enter cells, but he wasn’t involved in the current work.
The fact that SARS-CoV-2 targets nasal cells is not surprising, but it is important to know, says Stanley Perlman, an immunologist and microbiologist at the University of Iowa who studies coronaviruses. “Knowing which cells can be infected is the first step to knowing which cells are infected,” he adds.
The two studies are part of the Human Cell Atlas Lung Biological Network, an international consortium launched in 2016 that aims to characterize all the cells in the human body at a single-cell level. These efforts look at all of the tissues in the body using RNA sequencing (RNAseq) to find out which genes get expressed in different cell types in those tissues. For example, Alex Shalek, a chemist at the Massachusetts Institute of Technology and co-lead author of the Cell study, has been using single-cell RNAseq to study infectious and immunological conditions such as AIDS and tuberculosis, and chronic inflammatory diseases like asthma. When SARS-CoV-2 turned up this winter, his team and many other researchers in the network realized that they could mine their existing data sets to glean some biological insights into the new virus.
The researchers scoured that data looking for cells that expressed both ACE2 and TMPRSS2. Researchers currently think that the virus gets into cells when the spike protein that protrudes from its surface docks onto ACE2 on human cells. TMPRSS2, which is also located on human cell membranes, then cleaves the spike protein to activate it. The active spike protein can then fuse with the membrane to let the virus inside.
The two studies found that many cells that express ACE2 do not also express TMPRSS2. “It’s also important to know where TMPRSS2 is not present,” Farzan says. TMPRSS2 is not the only enzyme that can work with ACE2 to activate the spike protein, and the virus may be using alternative mechanisms to get into some cell types, he explains. Determining that will require knowing which cells actually get infected. If the virus is using other enzymes, then therapeutic strategies designed to inhibit TMPRSS2 might also have to block other enzymes as well.
The two papers also reported specific cell types in the lung, intestines, and cornea that express the ACE2-TMPRSS2 combo. “The really interesting thing is that not a lot of cells seem to express these two markers, yet you seem to see severe disease in some individuals,” Shalek says.
The research teams also uncovered some intriguing hints about how the innate immune response might be linked with the transmissibility of SARS-CoV-2. Shalek and his colleagues found that in epithelial cells—including cells lining the nose and lungs—ACE2 expression ramps up in the presence of type 1 interferon, a molecule released by immune cells that serves as the body’s first line of defense against viruses.
“Normally, the interferon response is helpful for controlling the virus, but in this case it also appears to increase the expression of ACE2,” which might have the opposite effect of giving the virus more targets to infect, Farzan says. The relationship between the receptor and immune molecule is not yet clear, Shalek says, but it is important to track because researchers are testing possible COVID-19 therapies that target type 1 interferon.
Lung Biological Network researchers are continuing to mine their datasets for further hints of SARS-CoV-2 pathology. A related study from the consortium, which is posted as a preprint on bioRxiv and is not yet peer reviewed, analyzes dozens of studies and single-cell datasets from the lung and other organs to parse out how age, gender, and smoking status affect the expression of ACE2, TMPRSS2, and other factors (2020, DOI: 10.1101/2020.04.19.049254). One intriguing finding is that children have few ACE2 receptors in their lower respiratory tract but strong ACE2 expression in their upper respiratory tract, including nasal cells, Farzan says. That may explain why they do not get as ill from COVID-19 as adults do, but suggests that they still have the potential to spread the virus.
Shalek and Sungnak note that the tissues used in all these studies were not infected by SARS-CoV-2, and it’s not clear how infection affects the expression of ACE2, TMPRSS2, and immune response genes. Researchers in their labs and others are already beginning to collect infected tissue to examine which cell types the virus penetrates and what happens when it does.
“One thing that these papers really point to is the amount of information that is available [and] sitting in our current databases,” Farzan says.



Join the conversation
Contact the reporter
Submit a Letter to the Editor for publication
Engage with us on Twitter