Advertisement
Grab your lab coat. Let's get started
Welcome!
Welcome!
Create an account below to get 6 C&EN articles per month, receive newsletters and more - all free.
It seems this is your first time logging in online. Please enter the following information to continue.
As an ACS member you automatically get access to this site. All we need is few more details to create your reading experience.
Not you? Sign in with a different account.
Not you? Sign in with a different account.
ERROR 1
ERROR 1
ERROR 2
ERROR 2
ERROR 2
ERROR 2
ERROR 2
Password and Confirm password must match.
If you have an ACS member number, please enter it here so we can link this account to your membership. (optional)
ERROR 2
ACS values your privacy. By submitting your information, you are gaining access to C&EN and subscribing to our weekly newsletter. We use the information you provide to make your reading experience better, and we will never sell your data to third party members.
Infectious disease
Covid-19
How do viruses leap from animals to people and spark pandemics?
Scientists want to understand how viruses like SARS-CoV-2 make these so-called zoonotic jumps to help spot the next big outbreak
by Alla Katsnelson, special to C&EN
August 30, 2020
| A version of this story appeared in
Volume 98, Issue 33

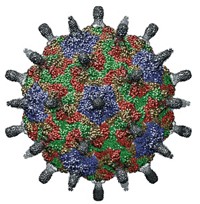
Credit: Yang H. Ku/C&EN/Shutterstock
In 2016, just as the worst Ebola epidemic in history was dying down in west Africa, researchers from a US government-funded pandemic-surveillance program called PREDICT sampled bats in the hardest hit region in search of Zaire ebolavirus, the virus responsible for the outbreak. They were looking for animal hosts from which the epidemic had sprung.
In brief
The SARS-CoV-2 pandemic has laid bare the urgent need for a better understanding of how viruses jump from animals to people, a process called zoonotic spillover. There are many hurdles a virus must get over to leap species to species, including finding a way to unlock receptors on the new host’s cell surfaces and learning how to replicate itself in those cells without alerting the host’s immune system. Scientists are working to better understand the molecular steps that viruses take to overcome these barriers. They hope to integrate that information with ecological surveillance of emerging zoonotic viruses to spot pathogens that could trigger a new outbreak.
Although they didn’t manage to do that, they found something else: a new species of ebolavirus, the genus of viruses that cause Ebola diseases. The new virus—the sixth in the genus to be identified—infects two bat species that roost in people’s homes in the Bombali region of Sierra Leone. The following year, the new virus popped up in the same bat species in Guinea and Kenya.
Although researchers don’t yet know whether this new Bombali virus infects people, or whether it would cause disease if it did, lab experiments suggest that it could. The protein that helps the Bombali virus, and the other five ebolaviruses, enter host cells binds to the correct receptor in lab-grown human cells to gain access to them, explains Tracey Goldstein, associate director of the One Health Institute at the University of California, Davis, who led the team that identified the new virus.
Support nonprofit science journalism
C&EN has made this story and all of its coverage of the coronavirus epidemic freely available during the outbreak to keep the public informed. To support us:
Donate Join Subscribe
The Bombali virus highlights an enigma for scientists monitoring the viruses that jump from wildlife to humans, a process called zoonotic spillover. Ebolaviruses, and many other viruses circulating in bats and other animals, “have that ability to spill over all the time,” Goldstein says. “But they don’t spill over all the time.”
The consequences can be significant when they do, as evidenced by the COVID-19 pandemic now gripping the world. Scientists are still trying to piece together exactly how SARS-CoV-2, the virus that causes COVID-19, spilled over from bats into humans. But, in general, whether or not a virus can make such a species leap and trigger an outbreak like COVID-19 depends on a complex dance between factors relating to ecology, viral evolution, and human immunity. Researchers are beginning to tease apart how these factors interact and how the molecular changes that viruses accrue as they evolve underlie that process. “That way, as we find viruses in wildlife, we can start to prioritize ones that look like they have the potential to be bad actors, and we can figure out where to focus to prevent a spillover event,” says Jonathan Epstein, vice president for science and outreach at EcoHealth Alliance.
Running the gauntlet
Scientists don’t know exactly how many different viruses exist in nature, but one recent estimate suggests that as many as 1.67 million still-unknown viruses infect mammals and birds, and that between 631,000 and 827,000 of those have the potential to make a zoonotic leap (Science 2018, DOI: 10.1126/science.aap7463). Even with estimating how many viruses could jump, “we have got no idea how many viruses out there are infecting humans,” says Raina Plowright, a disease ecologist and wildlife veterinarian at Montana State University. Novel viral infections might show up as encephalitis, a respiratory illness, or other symptoms in people living in remote parts of the world and never get diagnosed due to a lack of resources, Plowright says. As a result, many probably go unnoticed.
Regardless of the actual number, though, viruses that manage to jump species are rare—especially ones that do so successfully enough to cause large epidemics. “There are actually really effective barriers to zoonotic transmission,” Plowright says.

Many events must align for a virus to spill over and become established in people. First, the original host—the species that serves as the virus’s so-called reservoir—needs to rub elbows with people at a time when it is shedding enough virus for people to get exposed to a significant amount. Next, the virus has to be equipped with the molecular machinery to enter human cells. Specifically, it needs the right protein to bind to a receptor on a human cell, allowing it to slip inside. Then, it has to be able to replicate and to infect other cells, and while doing so, evade the human immune system.
Different viruses balance these factors differently, but the big-picture process is the same. “It’s the everyday, mundane, humdrum thing viruses do: they get into the cells, and they replicate, and they get out of the cells, and they infect [further cells],” says Edward Holmes, an evolutionary biologist at the University of Sydney. Along the way, they might pick up mutations or new genes that could help them make their way in another species.
Yet most potential spillover events “go nowhere,” Holmes says. In most cases, even if virus particles can infect a new host’s cells, they are effectively dead on arrival because they can’t replicate. Or, they might not make people ill, or might cause a small, local outbreak and then just burn themselves out because they lack the oomph to pass from person to person. “Very occasionally, they go ballistic,” like with SARS-CoV-2, Holmes says.
Spillover isn’t a lightning strike event—a once-and-done moment. It’s a lot less linear. Rather than considering a virus as a single entity with a static genome, it’s more accurate to think of “a whole spectrum of viruses that are variations on a theme,” Epstein says. “They’re a bunch of cousins that are genetically almost identical but different in ways that could really impact their ability to make that jump from their natural animal reservoir into people.” Virologists often refer to a collection of viruses—infecting one person or growing in one petri dish—as a swarm, says Michael Farzan, an immunologist at the Scripps Research Institute. Some members of the swarm might have genetic features that make them especially good at getting a grip on host receptors, or at efficiently replicating or transmitting from host to host.
Mastering that first spillover step—receptor binding—is paramount, because without it, the jump can’t happen. “The degree to which a virus uses the [host] receptor is a very good indicator for the degree to which the virus infects a particular species,” Farzan says.
Once a virus breaches that entry barrier, it must interact with dozens to hundreds of proteins in its new host to complete its life cycle while evading notice by the host’s immune system. Variation in even a single amino acid in its proteins can make or break the virus’s success.
Researchers know less about how viruses bypass these intracellular hurdles in a new host, but some viruses are yielding clues. For example, changes to influenza A proteins called PB1-F1, which induce inflammation in the host, affect a flu strain’s virulence. Meanwhile, HIV secured its jump to humans in part through wily tricks for evading our innate immune response. Because HIV sets up shop in a human host for the long term, Farzan says, integrating its genetic material into human DNA, HIV had to evolve a bag of sophisticated tricks to duck host-cell proteins called viral restriction factors that block viral replication.
Under pressure
For a virus to make a zoonotic jump, it must somehow pick up the equipment to infect a new host’s cells before it even comes across that host. But what pushes a virus to do that? Research on coronaviruses suggests that pressure from the virus’s current host can nudge it to accrue mutations that allow it to hijack hosts it hasn’t met yet.

For example, researchers have observed a molecular duel between some coronaviruses and bats. Coronaviruses like SARS-CoV-1, which caused the 2002–3 severe acute respiratory syndrome (SARS) epidemic, and SARS-CoV-2, use spike proteins on their surfaces to unlock receptors called ACE2 on the cells of their hosts. Several studies over the past few years have found that some of these bat coronaviruses can infect human cells, presumably because their spike proteins carry the right key to get into the cells via ACE2. More recently, bat biologist Zhengli Shi at the Wuhan Institute of Virology and her team looked at a bat species that carries these viruses (J. Virol. 2020, DOI: 10.1128/JVI.00902-20). They found that several of the viruses’ spike proteins can bind to human ACE2, supporting earlier work. But they also found that the bats themselves carried many different versions of ACE2. Some of the amino acid differences between the versions affected how well the virus spike protein could bind them.
The work suggests that evolutionary pressure acts on bat ACE2, pushing it to pick up mutations that prevent the coronaviruses’ spike proteins from binding. Those changes in turn put pressure on the viruses to pick up spike protein mutations to counter the bats’ ACE2 mutations. That pressure can select for mutations that coincidentally equip the virus to infect a new host.
“It’s pretty apparent that there’s this evolutionary arms race between the receptor binding domain and ACE2 that’s happening within the bats themselves,” says Tyler Starr, a postdoc in the lab of genome scientist Jesse Bloom at Fred Hutchinson Cancer Research Center. “Whatever it’s doing is ratcheting up this evolution and sometimes spitting out things that can bind potentially to many different ACE2s, including ours.”
In the case of the 2002–3 SARS outbreak, researchers could pinpoint viral sequences from bats and palm civets to conclude that SARS-CoV-1 likely jumped from bats to civets before reaching humans and infecting more than 8,000 people. Studies of the virus suggested that it had acquired two mutations that allowed it to bind tightly to human ACE2 and propagate within our cells, Farzan says. Both mutations were in the receptor binding domanin (RBD), which is the part of the spike protein that directly interacts with ACE2.
In 2004, the year after the epidemic ended, a handful of people in Guangzhou again caught the virus from a civet but only got mildly ill. When Farzan’s team sequenced the virus taken from one such person, they found that it carried only one of those two key mutations and consequently bound human ACE2 less tightly (EMBO J. 2005, DOI: 10.1038/sj.emboj.7600640). “Apparently, it was as a consequence not as transmissible,” Farzan says. “From there, we can make some guesses as to what was necessary for it to do really well in humans.”
Following SARS-CoV-2
In the case of SARS-CoV-2, the species route to humans is much less certain. Early on, researchers speculated that the virus may have jumped from horseshoe bats to pangolins before infecting humans. More recent thinking suggests that pangolins simply became infected the same way that humans did. Authors of a study published in July argued that the virus didn’t need to exchange genes in another animal after bats to allow it to infect humans, though that possibility can’t be ruled out (Nat. Microbiol. 2020, DOI: 10.1038/s41564-020-0771-4). “I’m not sure we will ever know what happened,” Montana State’s Plowright says.
Researchers speculate that two changes to the genome of a bat-infecting coronavirus made SARS-CoV-2 an effective human pathogen. The first was to adapt the RBD so it could bind to the human ACE. The second was to create a site in the virus’s spike protein that could be cleaved by a human cell enzyme called furin, which helps get the virus ready to enter a cell. Such furin-binding sites are present in other coronaviruses but don’t generally appear in ones like SARS-CoV-1 and SARS-CoV-2.

So far, though, efforts to find other mutations that might power the virus’s pandemic prowess have largely fallen short. Starr, Bloom, and their colleagues set out to mutate every position in the 201-amino-acid RBD one by one and then examine how each mutation affects the protein’s folding pattern and capacity to bind ACE2. They found that the region has a high tolerance for mutations. “It can handle a high number of mutations and do its job just fine,” Starr says. The team even found dozens of mutations that boosted the RBD’s ability to bind the ACE2 receptor, but the virus seems to have not adopted any of them (Cell 2020, DOI: 10.1016/j.cell.2020.08.012).
That finding suggests that the virus functions effectively with the binding affinity it has, and that there’s no strong selective pressure pushing for mutations that might increase it, Starr says. He wonders if that’s because the virus is tearing through a population that has never encountered it and has no immune defenses against it. “Right now, the virus has basically found a buffet table of susceptible [hosts].”
Advertisement
As the COVID-19 pandemic has progressed, one virus mutation does appear to have become a permanent feature of SARS-CoV-2’s genome. Researchers collecting virus samples from infected patients have been sequencing viral genomes and analyzing the strains spreading in different parts of the world. They have found that one mutation, a change from an aspartic acid (D614) to a glycine (G614), is now present in the majority of SARS-CoV-2 viral sequences. People infected with strains carrying this mutation tend to shed more virus than those infected with strains that don’t, hinting that this mutation may make the virus more infectious (Cell 2020, DOI: 10.1016/j.cell.2020.06.043). Farzan’s team has conducted cell studies with the lab-made viruses carrying SARS-CoV-2 spike proteins and found that the mutation causes the virus to more readily infect human cells, perhaps because there are more spike proteins on the virus’s surface (bioRxiv 2020, DOI: 10.1101/2020.06.12.148726v1). The data from those studies have not yet been peer reviewed.
However, how much this mutation is ratcheting up the virus’s potency—and how exactly it affects its spread—is still up for debate. Holmes says that although the shift likely does make the virus somewhat more transmissible, it probably spread so widely because it made its appearance in Europe early in the pandemic and got swept up in the transmission chain in Italy, where so many people were infected in a short amount of time and then traveled across the globe. “It’s the epidemiology that has driven that, not the evolution of the virus,” he says.
Spotting the next jump
Researchers still have much to learn about SARS-CoV-2’s zoonotic leap—and how to prevent viral spillover in general. For the past decade, UC Davis’s Goldstein, EcoHealth Alliance’s Epstein, and other collaborators working on PREDICT have collected samples from wildlife and people in areas where outbreak risks are high. Shi and her colleagues at the Wuhan Institute of Virology, working with PREDICT, reported in 2018 that people living close to caves where bats carrying different SARS coronaviruses live have antibodies to such coronaviruses, though it’s impossible to pinpoint which viruses in particular (Virol. Sin. 2018, DOI: 10.1007/s12250-018-0012-7).

Goldstein and her colleagues now plan to go back to blood samples that they’ve collected from people in Cambodia, Vietnam, and Myanmar, to see if people in communities that have high exposure to bats have more such antibodies than people in communities that don’t. By identifying regions where exposure is high, researchers can study how people and animals come into contact and try to pinpoint behaviors that would decrease it, Goldstein says.
Using humans as a filter is a powerful way to narrow in on especially concerning regions where potentially zoonotic viruses are endemic, Plowright says. She is also taking another approach: looking for viruses with spillover potential by looking at the microbes themselves. She is collaborating with researchers at Cornell University to screen viruses collected through surveillance projects for zoonotic potential by running lab tests to determine whether they can infect human cells. The team has been running the screen on henipavirus samples collected in Bangladesh and Australia and are now beginning to test coronaviruses. “Of course, there’s a lot more to zoonotic infection than a cell culture,” she says. But the screen provides a way to identify potentially dangerous viruses for further study.
Ultimately, however, monitoring for spillover will require scientists to gain a much better ecological picture of the regions in which potentially dangerous viruses are endemic. When PREDICT sunsets this year, other efforts such as the Global Virome Project, a 10-year collaboration launched in 2018, will continue crucial surveillance work. But what researchers most need to develop, Plowright says, is a long-term understanding of ecological changes in hot spots.
For example, she is working with collaborators in Australia who have spent 24 years tracking a bat population that carries henipaviruses, which tend to be highly pathogenic when they infect people. The bats used to be almost entirely nomadic, traveling among patches of native forest, but now as critical habitat is disappearing, they are moving into areas where people live.
Understanding the ecological dynamics of the zoonosis for these viruses could point to specific remedies like replanting forests. They could also reveal circumstances, such as stress, that may cause bats that carry potentially dangerous viruses to shed them more readily.
“The problem is, we don’t have data on so many of these events,” Plowright says. As people encroach on wilderness areas with lots of biodiversity, they expose themselves to the biggest requirement for zoonotic spillover—proximity to animal carriers of potentially dangerous viruses. By learning more about the ecological role in zoonosis, scientists could find new ways to slow or prevent spillover. In terms of spending resources to help us spot the next virus that could make a species jump and spark a pandemic, she says, “That’s where I would invest.”
Alla Katsnelson is a freelance writer based in Massachusetts.




Join the conversation
Contact the reporter
Submit a Letter to the Editor for publication
Engage with us on Twitter