Advertisement
Grab your lab coat. Let's get started
Welcome!
Welcome!
Create an account below to get 6 C&EN articles per month, receive newsletters and more - all free.
It seems this is your first time logging in online. Please enter the following information to continue.
As an ACS member you automatically get access to this site. All we need is few more details to create your reading experience.
Not you? Sign in with a different account.
Not you? Sign in with a different account.
ERROR 1
ERROR 1
ERROR 2
ERROR 2
ERROR 2
ERROR 2
ERROR 2
Password and Confirm password must match.
If you have an ACS member number, please enter it here so we can link this account to your membership. (optional)
ERROR 2
ACS values your privacy. By submitting your information, you are gaining access to C&EN and subscribing to our weekly newsletter. We use the information you provide to make your reading experience better, and we will never sell your data to third party members.
Microbiome
Gut bacteria feast on the pills we pop
Mounting data raise the question: How will drug firms respond?
by Megha Satyanarayana
August 31, 2019
| A version of this story appeared in
Volume 97, Issue 34

Matthew Redinbo remembers the day he entered the murky waters of the gut microbiome. He had popped in to say hi to Lisa Benkowski, a colleague in the Chemistry Department at the University of North Carolina at Chapel Hill. It was 2002, Benkowski had colon cancer, and she was taking a powerful chemotherapy called irinotecan.
“She said the side effects were a nightmare,” Redinbo says, describing how a large number of people on the drug, marketed as Camptosar, suffer from diarrhea and nausea. “Some days she could not get out of bed and certainly could not leave the house.”
Their conversation stayed with him. Why were irinotecan’s side effects so debilitating? Could they be prevented? The answers, Redinbo would find out, were hidden in the bacteria in our intestines.
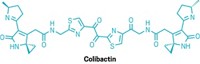
As they study microbiome-drug interactions, researchers are learning not only that intestinal microbes dine on a great many of the small-molecule drugs that we take—those like irinotecan—but also that what the microbes are doing to those drugs may affect whether they work and whether they are safe. Yet with rare exceptions, we still know little about how these bugs slice and dice our medications and what happens to the fragments they leave behind. The reactions happening within our guts could reshape the way drugmakers create and test medicinal compounds.
“I’ve talked to a couple of companies about what I can do to help them test stuff, and then I don’t hear from them again,” says Nichole Klatt, a researcher at the University of Miami who has found that vaginal microbes deactivate HIV drugs. “So, do they care? I don’t know. Should they care? I think definitely yes because I think this has a much bigger impact on human health than people ever could have imagined.”
Bugs ’n’ drugs
Some of the first reports that fecal bacteria could break down drugs came in the 1940s and ’50s. But for a long time afterward, the scientific literature went kind of dark on that topic, Redinbo says. Many scientists studying metabolism suspected that the liver and the bacteria in our guts were involved in drug metabolism. But advances in human genetics and cloning allowed them to drill down into the liver’s majority contribution to drug metabolism, and focus shifted more toward the human cell side of drug breakdown.
Still, scientists didn’t abandon the microbiome. Rather, industry scientists who studied pharmacokinetics—how the body metabolizes drugs—weren’t publishing their findings, Redinbo says.
“I would go to meetings and present my work, and there was invariably a seasoned drug metabolism expert who would pull me aside and say, ‘We’ve known this for decades,’ ” Redinbo says. These experts would tell him they had detected in human plasma and other fluids metabolites that humans themselves couldn’t make. But they didn’t report the metabolites, he says, because they had no idea how the molecules were generated. The gut seemed like a black box.
Research on the gut microbiome has exploded in the past 15 or so years, in part because of high-throughput technologies and computing power that have allowed scientists to test vast numbers of samples and to distinguish among hundreds of bacterial species in our intestines relatively quickly. And with these advances has come a burst of data showing how prevalent the interactions between gut microbes and drugs can be. For example, in 2018, a group of researchers in Japan and Germany demonstrated that about one-quarter of 1,200 mostly generic drugs, covering all major therapeutic classes except for antibiotics, quelled microbes in the human gut (Nature, DOI: 10.1038/nature25979).
And then there are all the things that gut microbes are doing to drugs.
Libusha Kelly, a microbiome scientist at Albert Einstein College of Medicine, says that gut microbes are tiny chemists, carrying out a vast array of reactions, such as hydrolysis, deamination, dealkylation, demethylation, and acetylation. Her lab’s most recent work tries to predict how microbes will chop up different drugs.
“There’s a tremendous amount of chemistry that the gut microbiome can do that’s relevant to drugs,” she says.
Recent tests carried out by Andrew Goodman and his team at Yale University support this sentiment. Similar to Kelly, the researchers are trying to predict whether gut microbes will digest a drug. They examined 271 popular small-molecule drugs and found that dozens of common gut microbes were able to digest about two-thirds of them. Through mass spectrometry, Goodman’s team was able to identify not only the metabolites produced by the microbes but also the chemical features these bacteria like to chow down on: lactones, azo groups, nitro groups, and urea groups (Nature 2019, DOI: 10.1038/s41586-019-1291-3).
Goodman says his team still doesn’t know how to interpret some of these findings because the majority of drug metabolism happens in the small intestine, and it’s not a place rife with microbes. Most of our microbes are in the large intestine. Some of what Goodman and his team are seeing in their experiments in mice and petri dishes might not have the opportunity to happen in a person’s gut.
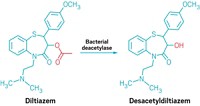
While Goodman and others have focused on broad analyses of drug-bug interactions, other researchers have looked at the effects of bacteria on individual drugs. These scientists are trying to understand not only what microbes are doing to a drug but also what happens after the drug is cleaved by bacterial enzymes. Take, for example, irinotecan, which stops cancer cells from dividing. After someone takes an irinotecan pill, the compound is absorbed into the bloodstream via the digestive tract, and it travels to the site of the tumor. But as it courses through the blood, irinotecan also finds its way to the liver, where it is deactivated by liver enzymes to prevent it from doing any damage to the rest of the body. To deactivate the compound, the liver enzymes decorate it with a sugar molecule.
However, once the sugar-speckled drug gets to the intestines, bacteria scavenging for energy pluck the sugar off, and irinotecan becomes active again, Redinbo says (Science 2010, DOI: 10.1126/science.1191175).
In many places in the body, this sugar-stripping chemical reaction wouldn’t matter—not all healthy cells are actively dividing, so irinotecan likely wouldn’t affect them. But the intestine has a cache of stem cells that help it renew its lining every couple of days. Irinotecan kills these cells, which are dividing, Redinbo says, and this leads to the diarrhea and other gastrointestinal side effects that sidelined his colleague Benkowski. Because of these side effects, oncologists must limit the amount of the drug they administer, lowering the efficacy of the cancer treatment.
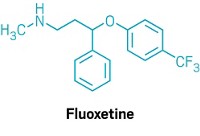
The limitations that doctors face because of bug-drug interactions aren’t just with cancer therapies like irinotecan. People with Parkinson’s disease often have low dopamine in parts of their brains that are associated with motor function. They are usually prescribed a drug called levodopa, a source of dopamine, to reduce their tremors and shakiness.
Dopamine itself can’t cross the blood-brain barrier, but levodopa can. Once levodopa is inside the brain, enzymes decarboxylate it, unleashing active dopamine, says Harvard University chemist Emily Balskus. To prevent premature decarboxylation outside the brain, levodopa is given in combination with other drugs that prevent the reaction. But scientists have noted that even with the added decarboxylase inhibitors, levodopa still works inconsistently from person to person, Balskus says. Scientists began to wonder if gut microbes and their enzymes were involved.
Balskus and Peter Turnbaugh at the University of California, San Francisco, investigated and found that two species of common gut microbes hack bits off levodopa sequentially, first creating dopamine and then producing a molecule called m-tyramine. Turnbaugh says there is some evidence that m-tyramine causes intestinal side effects.
Yet some are skeptical that these bug-drug reactions amount to anything clinically relevant. The idea that the intestines matter in drug metabolism is still somewhat controversial, Turnbaugh says. “There is a general challenge in just trying to bring people together” in their thinking.

Quirky peaks
Scott Obach is running late.
“I totally got caught up with something in the lab and forgot,” he tells C&EN later in the day after having to miss an earlier interview. The Pfizer scientist is among the world’s experts on how the human body metabolizes drugs, and he sometimes loses himself in his work. At the pharma giant, he’s responsible for characterizing the absorption, distribution, metabolism, and excretion (ADME) of drug candidates.
It’s not that industry isn’t interested in what gut microbes are doing to drugs, he says. It’s just too soon to act. Blame the lack of technology. Blame the relative dearth of data. Blame the cost and time that overhauling R&D would entail. But for now, “it’s not a concern,” Obach says.
To test how the body metabolizes a drug candidate, Obach says, healthy volunteers take small doses of a radioactively labeled version of the candidate and, over the course of several hours, have their blood, urine, and feces monitored by mass spectrometry as their bodies break it down. The readout is a series of peaks that correspond to various metabolites, pointing to where—and sometimes through what class of reaction—bonds in the drug candidate were severed.
The liver does most of the work to break down drugs with enzymes, Obach says, but enzymes in our blood, as well as in our intestines, contribute to metabolism too. Exactly how much the enzymes in our intestines contribute to the process isn’t measurable with standard industry ADME analytical tools.
When his team looks at its mass spec results, Obach says, the scientists will sometimes see quirky mass spec peaks. Those odd peaks could be bacterial in origin, he says. But he also says he’s recently learned that some of the peaks that people thought were “normal,” arising from mammalian cell metabolism, may actually stem from bacterial metabolism. The bacterial and mammalian cell metabolism pathways are similar enough that they create similar products. Current technology can’t distinguish between what mammalian cells contribute to an individual peak and what bacterial cells contribute.
Bacterial metabolism “may be an overlooked contributor in some cases, and we probably need to have more diligence in the future to understand it,” Obach says. Until it’s better understood, he adds, not much will change in the way he does his work.
Other companies are also adopting a wait-and-see attitude.
Henry Haiser is a microbiome scientist who recently left Novartis. Before joining industry, Haiser was part of Turnbaugh’s team at UCSF and demonstrated that a specific microbe could digest a common heart failure drug called digoxin, which doesn’t work in some people.
Haiser points out that some companies are examining how approved immunotherapy drugs interact with the gut microbiome. But he says that when it comes to early stages of drug development, a lot of companies are hesitant to make any big changes where the microbiome is concerned.
Haiser says that while he was at Novartis, a scientist working on drug metabolism studies would occasionally have a wonky result and collaborate with him to chase down whether the microbiome was involved. But these were one-off experiments, he says. There was never a systematic effort to address microbiome-drug interactions.
Haiser will soon join Takeda Pharmaceuticals USA and expects that for the time being, bug-drug experiments will be more about answering specific questions in the development of a single compound rather than broad questions about how to choose the best compound to pursue clinically.
Advertisement
Obach says the team at Pfizer is investigating ways to test for microbiome interactions during ADME, but he thinks it will be a decade or longer before bacterial metabolism tests will trickle down into routine drug development.
“It will continue to be used as a problem-solving or an issue-resolving set of experiments, where clinical observation is made and you need to respond to it, but as for its routine incorporation into the drug discovery setting, it’s too early,” he says.
Sooner rather than later
Even though what we now know about the microbiome’s influence over drug metabolism isn’t going to change drug development immediately, Turnbaugh and others think the impact will be felt sooner than in 10 years.
For instance, Turnbaugh and Balskus have reported a new small-molecule inhibitor that blocks the bacterial enzymes that cleave levodopa and transform it into m-tyramine (Science 2019, DOI:10.1126/science.aau6323). And Redinbo is nearing clinical trials for a small-molecule inhibitor that prevents bacterial enzymes from reactivating irinotecan by lopping off its protective sugar (Science 2010, DOI: 10.1126/science.1191175). Targeting bacterial enzymes is probably the most tangible way to combat what these researchers see as a devastating and unnecessary loss of drug efficacy that could be more widespread than we currently know.

Redinbo was never able to tell Benkowski what he learned—she died soon after their conversation. And when his group published its paper about the small-molecule inhibitor several years later, he dedicated it in part to her.
Redinbo says he firmly believes that what we learn about gut microbes and drug metabolism will at some point lead to a doctor ordering rapid microbiome testing before prescribing a drug like levodopa or irinotecan. Regulatory bodies will likely favor this approach—testing before prescribing—over incorporating microbiome testing into the drug development process because the latter might be more cumbersome.
Yet for some microbiome researchers, testing before prescribing isn’t enough. Bug-drug interaction testing should be incorporated into drug development as soon as possible, they argue.
Klatt, the HIV researcher at the University of Miami, has found that some HIV drugs are metabolized by vaginal microbes. One in particular is dapivirine, a therapeutic released from vaginal rings that is nearing Phase III tests as an HIV preventive for teens and young women in parts of Africa, including South Africa. Klatt says earlier trials found the ring reduced the risk of HIV infection by only about 30%, and she believes the groups running the trials should consider whether dapivirine is the right drug to use in a vaginal ring.
“These are the girls that are at the highest risk of HIV infection, and I think it’s downright unethical because the people running this trial know this,” Klatt says, explaining that the low efficacy means that women in the trial who might otherwise be on more effective preventives could get infected.
For now, the trials continue, and the next phase will include an investigation of the vaginal microbiomes of the women enrolled, says spokesperson Lisa Rossi of the Microbicide Trials Network, the group helping coordinate the trials. Rossi says that the group has seen no clinical evidence that vaginal bacteria identified by Klatt do anything to dapivirine. But, as researchers learn more about how our microbes metabolize drugs, concerns such as the one raised by Klatt may become more common.


Join the conversation
Contact the reporter
Submit a Letter to the Editor for publication
Engage with us on Twitter