Advertisement
Grab your lab coat. Let's get started
Welcome!
Welcome!
Create an account below to get 6 C&EN articles per month, receive newsletters and more - all free.
It seems this is your first time logging in online. Please enter the following information to continue.
As an ACS member you automatically get access to this site. All we need is few more details to create your reading experience.
Not you? Sign in with a different account.
Not you? Sign in with a different account.
ERROR 1
ERROR 1
ERROR 2
ERROR 2
ERROR 2
ERROR 2
ERROR 2
Password and Confirm password must match.
If you have an ACS member number, please enter it here so we can link this account to your membership. (optional)
ERROR 2
ACS values your privacy. By submitting your information, you are gaining access to C&EN and subscribing to our weekly newsletter. We use the information you provide to make your reading experience better, and we will never sell your data to third party members.
Neuroscience
Denali’s clinical data shows promise of blood-brain barrier shuttles
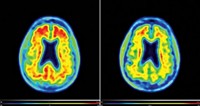
New technologies that can smuggle large biologic drugs into the brain may open up new therapeutic opportunities
by Asher Mullard, special to C&EN
February 12, 2021

Denali Therapeutics has found a way to sneak biologics past the blood-brain barrier (BBB), suggests preliminary Phase I data of the firm’s DNL310 in Hunter syndrome.
Hunter syndrome is a rare, lysosomal storage disorder caused by mutations in iduronate 2-sulfatase (IDS), an enzyme that degrades sugar molecules called glycosaminoglycans. People with the disease are typically treated with Takeda’s enzyme-replacement therapy idursulfase, but this biologic can’t cross the BBB and so most patients still suffer from progressive cognitive decline brought on by the accumulation of glycosaminoglycan in the brain.
Denali’s BBB-bypassing candidate DNL310 consists of the IDS enzyme fused to a protein fragment that binds the transferrin receptor—a carrier protein that is found in the cells that make up the blood vessels that feed the brain. This "trojan horse" approach hijacks the receptor to carry a therapeutic, rather than just iron, into the brain.
The preliminary results covered 5 boys treated weekly with intravenous DNL310. By 3 months, cerebrospinal fluid (CSF) levels of a key glycosaminoglycan fell on average by 85%, returning to normal or near normal levels, the company reported at the WORLDSymposium. Glycosaminoglycan levels also fell in the urine, suggesting DNL310 is active outside the brain too.
“It’s very impressive data,” says University of Washington professor William Banks, who studies the BBB. “To see those kinds of changes in the CNS is really very helpful.”
Although the drop in sugar molecules is encouraging, Denali will still need to prove the treatment can prevent or slow cognitive decline.
Other companies have attempted to address the cognitive effects of Hunter Syndrome, but their treatments floundered in late-stage studies. In 2015, a Phase 1/2 trial of intrathecal idursulfase (IT-idursulfase), wherein the enzyme replacement is delivered directly into the CSF by lumbar puncture, lowered CSF glycosaminoglycans levels by 90%. But a Phase 2/3 trial of this drug failed to show that the therapy slowed cognitive decline. Takeda acquired this drug in 2018, via its purchase of Shire. It is still hoping for an FDA approval later this year, noting that subsequent analyses suggested the drug benefited patients who started treatment before the age of 6.
Denali is unfazed by the setback for intrathecally-delivered enzyme-replacement therapy. Whereas IT-idursulfase diffuses into the brain from a lumbar puncture in the lower spine, intravenously dosed DNL310 gains access through a 600km network of small capillaries that surround the brain. As such, the biodistribution of DNL310 will be better, says Denali’s chief medical officer and head of development, Carole Ho.
Preclinical and clinical findings back that up, she adds. “We have additional biomarker data that tells us that we’re doing something differently, and that we are having an effect on lysosomal function,” says Ho.
Denali plans to start a larger trial of DNL310 in 2022.
These early results have good implications for Denali’s technology, says Denali CEO Ryan Watts. “Getting the molecule into the brain, no overt immunogenicity and sustained responses: those should read through for all our transport vehicle programs,” he says.
Denali plans to advance two more BBB-busting therapeutics into the clinic by early next year—one for frontotemporal dementia and the other for Alzheimer’s disease. Denali has partnered with Takeda on both of these candidates. The biotech firm is also in the process of picking an antisense oligonucleotide-shuttle program to advance.
A few other companies are also testing similar BBB shuttle technologies in the clinic. JCR Pharmaceuticals has filed for regulatory approval in Japan for its pabinafusp alfa, IDS fused to an antibody that binds the transferrin receptor, also for Hunter Syndrome. Roche’s RG6102, an anti-amyloid antibody fused to transferrin-binding shuttle, is in a Phase I Alzheimer trial.
Correction
This story was updated on Feb. 16, 2021, to correct Carole Ho's title and clarify the mechanism of action of Denali's drug. Ho is Denali's chief medical officer, not chief scientific officer; she is also head of development. And the transferrin receptor carries Denali's drug and iron, not just the drug, across the blood-brain barrier.




Join the conversation
Contact the reporter
Submit a Letter to the Editor for publication
Engage with us on Twitter