Advertisement
Grab your lab coat. Let's get started
Welcome!
Welcome!
Create an account below to get 6 C&EN articles per month, receive newsletters and more - all free.
It seems this is your first time logging in online. Please enter the following information to continue.
As an ACS member you automatically get access to this site. All we need is few more details to create your reading experience.
Not you? Sign in with a different account.
Not you? Sign in with a different account.
ERROR 1
ERROR 1
ERROR 2
ERROR 2
ERROR 2
ERROR 2
ERROR 2
Password and Confirm password must match.
If you have an ACS member number, please enter it here so we can link this account to your membership. (optional)
ERROR 2
ACS values your privacy. By submitting your information, you are gaining access to C&EN and subscribing to our weekly newsletter. We use the information you provide to make your reading experience better, and we will never sell your data to third party members.
Neuroscience
Genetic glitch may forestall Alzheimer’s
Researchers aim to develop new therapies that mimic the mutation’s effects
by Alla Katsnelson, special to C&EN
November 5, 2019
| A version of this story appeared in
Volume 97, Issue 44

A rare mutation may protect people with a familial form of early-onset Alzheimer’s disease from developing it. The mutation, located in the gene APOE3, hampers how its protein binds with sugars that play a role in the disease. Targeting this process might yield novel therapies, the researchers say (Nat. Med. 2019, DOI: 10.1038/s41591-019-0611-3).
Researchers discovered the apparently protective mutation when studying people within an extended family in Medellín, Colombia, who carry a mutation in a different gene, called presenilin 1 (PSEN1). About half of those who carry the PSEN1 mutation develop early signs of the disease by their mid-40s and dementia by around age 50.
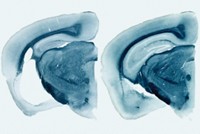
During their research, scientists encountered one woman who stood out: although she carried the PSEN1 mutation and was in her 70s, she had only mild cognitive impairment. What’s more, the woman’s brain also had high levels of clumped proteins called amyloid plaques, a characteristic sign of Alzheimer’s. Though she had more amyloid plaques than people with the PSEN1 mutation who develop the disease in their 40s, she had few symptoms.
“That was surprising,” says Joseph Arboleda-Velasquez, a cell biologist at Harvard Medical School and one of the study’s authors. “It shows that even if you have a lot of amyloid it is still possible to block the cascade that leads to pathology.”
In search of an explanation, Arboleda-Velasquez and his team sequenced the woman’s genome. This led them to APOE3, a version of a protein called APOE. APOE protein combines with lipids to make lipoproteins, and some variations of it affect a person’s risk of developing Alzheimer’s. A variation called APOE4 raises the risk of developing Alzheimer’s; APOE2 lowers it. APOE3, the most common APOE variation, is thought to be neutral for Alzheimer’s. The Medellín woman has APOE3, with a twist.
Both copies of the woman’s APOE3 gene have a very rare glitch called the Christchurch mutation, which is known to interfere with how cells metabolize lipids but has not previously been studied in the context of Alzheimer’s. Researchers have never seen it in combination with the PSEN1 mutation.
The Christchurch mutation is known to affect the region of the APOE3 protein that binds to a class of sugars called heparan sulfate proteoglycans, which have been implicated in the pathology of Alzheimer’s disease. In the disease, these sugars bind to the toxic protein tau and help it spread. So the researchers looked at how the mutant APOE3 proteins interact with these proteoglycans, using affinity chromatography to test how well they bound together.
Compared with wild-type APOE3 proteins, mutant APOE3 protein didn’t bind well to these sugars. “That gave us a lot of encouragement that maybe this was the likely mechanism” for the mutation’s protective effect, says Arboleda-Velasquez. The researchers speculate that by thwarting the APOE protein’s interaction with the proteoglycans, the Christchurch mutation throws a wrench in the cellular cascade of events that causes dementia in Alzheimer’s disease.
Arboleda-Velasquez says drugs that modulate this interaction might be useful for treating the disease. As a first test of the idea, the researchers created an antibody that recognizes the section of APOE3 that contains the Christchurch mutation and found that it hinders the interaction between the proteoglycan heparin and a normal APOE3 protein, mimicking the effect of the mutation.
“This is an excellent, thought-provoking, hypothesis-generating study,” says Michael Greicius, a neurologist at Stanford University, who was not involved in the work. However, he says, the conclusion that the Christchurch mutation deploys a protective mechanism would be more convincing if people in the PSEN1 family with just a single version of it were partially protected from developing dementia. Out of 117 family members, seven people had a single copy of the gene. The Medellín woman was the only person in the study who had both.
Arboleda-Velasquez says his team is now studying people with a single copy of the APOE3 mutation in more depth to explore how the mutation exerts its protective effects.



Join the conversation
Contact the reporter
Submit a Letter to the Editor for publication
Engage with us on Twitter