Advertisement
Grab your lab coat. Let's get started
Welcome!
Welcome!
Create an account below to get 6 C&EN articles per month, receive newsletters and more - all free.
It seems this is your first time logging in online. Please enter the following information to continue.
As an ACS member you automatically get access to this site. All we need is few more details to create your reading experience.
Not you? Sign in with a different account.
Not you? Sign in with a different account.
ERROR 1
ERROR 1
ERROR 2
ERROR 2
ERROR 2
ERROR 2
ERROR 2
Password and Confirm password must match.
If you have an ACS member number, please enter it here so we can link this account to your membership. (optional)
ERROR 2
ACS values your privacy. By submitting your information, you are gaining access to C&EN and subscribing to our weekly newsletter. We use the information you provide to make your reading experience better, and we will never sell your data to third party members.
Neuroscience
How modified Chantix and a bioengineered ion channel may help diseases like epilepsy and depression
The new technique could help neuroscientists study the brain as well as offer targeted therapies for neurological disorders
by Megha Satyanarayana
March 15, 2019

Some neurological disorders, like chronic pain, depression, and epilepsy, are caused in part by an imbalance in neurochemical signals that either excite or calm down neurons. Existing treatments try to restore neurochemical balance, but these drugs not only act on the neurons involved in the disease, but also unrelated ones, leading to unwanted side effects.
To try and make more precise treatments, researchers led by chemical biologist Scott Sternson of Howard Hughes Medical Institute’s Janelia Research Campus have created what they call a chemogenetic system that allows them to control the activity of specific small groups of brain cells through an engineered ion channel that responds to a small molecule of their design (Science 2019, DOI: 10.1126/science.aav5282). In tests in mice and a single monkey, the researchers could activate specific neurons simply by feeding the animals their designed compound.
Experts think the work could not only have therapeutic potential, but also could help neuroscientists study the brain by providing a simple way to analyze the role of specific sets of neurons in living animals. Current methods to do so, like brain stimulation or optogenetics, are more invasive and require complex machinery.
“I think it’s going to be a big deal, this as a new therapeutic approach,” says Rebecca Seal, a neuroscientist at the University of Pittsburgh who is using a similar chemogenetics system to study chronic pain.
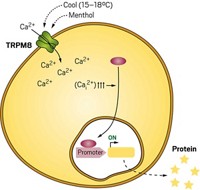
To create the chemogenetic system, Sternson’s lab first pieced together an ion channel from the parts of existing ones. They took a modified ligand binding domain from an acetylcholine receptor and the ion-conducting pore from a channel involved in the vomit response. Their plan was to create a channel that, when turned on by the binding of a small molecule, would allow a flow of cations into a neuron, triggering the cell to release neurotransmitters. They also created other ion channels that shuttle chloride ions.
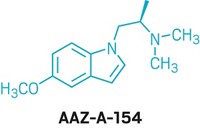
The team then looked for molecules that could turn on their ion channel. They tested various drugs approved by the US Food and Drug Administration on the engineered channel, a choice, Sternson says, that could make it easier to overcome regulatory barriers as the technique moves toward the clinic. The best performing molecule was varenicline, the active ingredient in the smoking-cessation drug Chantix. The researchers tinkered with the compound to improve its specificity for the engineered ion channel and eventually created an analog, 817, which has one of the most potent and effective interactions with a receptor recorded to date, Sternson says. A small dose of the analog produces a robust response from the ion channel.
To test the channel in animals, the team needed to get the it into the brain. They used a viral delivery system that delivered the genes for the channel to specific cells in the brains of mice and a monkey. Once the target cells started making the ion channels, the team gave the animals their varenicline analog. The scientists used imaging and electrical recording to monitor the activity of the neurons and found that the molecule had activated them.
Advertisement
Sternson says that the low dose of drug required to activate the ion channels and the success in getting the channels into the brain helps set the stage for future experiments to validate the system for potential medicinal use.
“This system is what we think is the best system out there for extending chemogenetics to people,” Sternson says.
While the chemistry is impressive, “whether the engineered channels will be safe in a clinical setting is unclear,” says Bryan Roth, a pharmacologist at the University of North Carolina School of Medicine. Roth invented designer receptors exclusively activated by designer drugs, or DREDDs, which use chemogenetic techniques to engineer other receptors, including G-protein coupled receptors.
Sternson has started a company to further investigate the therapeutic potential of the method and is using the system to understand neurobiological processes like hunger.


Join the conversation
Contact the reporter
Submit a Letter to the Editor for publication
Engage with us on Twitter