Advertisement
Grab your lab coat. Let's get started
Welcome!
Welcome!
Create an account below to get 6 C&EN articles per month, receive newsletters and more - all free.
It seems this is your first time logging in online. Please enter the following information to continue.
As an ACS member you automatically get access to this site. All we need is few more details to create your reading experience.
Not you? Sign in with a different account.
Not you? Sign in with a different account.
ERROR 1
ERROR 1
ERROR 2
ERROR 2
ERROR 2
ERROR 2
ERROR 2
Password and Confirm password must match.
If you have an ACS member number, please enter it here so we can link this account to your membership. (optional)
ERROR 2
ACS values your privacy. By submitting your information, you are gaining access to C&EN and subscribing to our weekly newsletter. We use the information you provide to make your reading experience better, and we will never sell your data to third party members.
Biomaterials
Genetically-engineered malaria vaccines show promise in the clinic
Inoculating people with weakened parasites may generate stronger immune response than the current malaria vaccine
by Mark Peplow, special to C&EN
May 21, 2020
| A version of this story appeared in
Volume 98, Issue 20
Two experimental malaria vaccines have delivered promising results in first-in-human trials, demonstrating how genetic engineering is driving a new wave of vaccines that could protect people from this killer disease.
The World Health Organization estimates that there are more than 200 million cases of malaria each year, causing almost half a million deaths. Although malaria can be treated with drugs, researchers have spent decades trying to develop vaccines that could prevent and potentially even help eradicate malaria. In 2019—after 32 years of development and clinical trials—a vaccine called Mosquirix (also known as RTS,S) was finally rolled out to young children in pilot programs across three African countries.
Mosquirix acts against the most deadly form of human malaria, caused by the parasite Plasmodium falciparum. It is the only malaria vaccine to move beyond Phase 3 clinical trials, but it is no silver bullet. The vaccine only prevents about 40% of malaria cases, and the protection wanes after a few years. More than 20 other vaccines, which are still moving through the development pipeline, aim to improve on that performance.
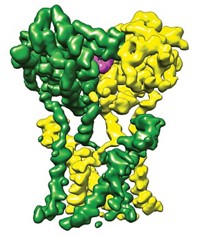
One of the big challenges for these vaccines is that malaria parasites have a very complex life cycle, shape-shifting as they move through mosquitoes and human hosts. Mosquirix tackles the parasite when it is a sporozoite—the form that mosquitoes inject into their victims’ bloodstreams, and which then infects liver cells. The vaccine contains a circumsporozoite protein (CSP) that induces the human body to generate antibodies against sporozoites.
Two new vaccines also target the liver stage, but contain whole sporozoites that have been attenuated—they are alive, yet unable to cause malaria. Since sporozoites carry dozens or hundreds of proteins that could trigger an immune response, researchers think the two vaccines may offer more robust protection than the lone CSP in Mosquirix.
The first vaccine, PbVac, uses Plasmodium berghei, a relation of P. falciparum that infects rodents but does not cause disease in humans. “The parasite is naturally attenuated, so it’s inherently safe in that way,” says Miguel Prudêncio at the University of Lisbon, part of the team behind PbVac. The researchers genetically modified P. berghei sporozoites to express P. falciparum CSP.
Volunteers who were treated with PbVac and then infected with malaria had, on average, a 95% reduction in P. falciparum in their livers. In vitro tests showed that the vaccine triggered an antibody response that stopped sporozoites entering liver cells (Sci. Transl. Med. 2020, DOI: 10.1126/scitranslmed.aay2578). Prudêncio says that it should be possible to further engineer P. berghei sporozoites to carry other antigens in addition to CSP.
The second vaccine, PfSPZ-GA1, was developed by a team in the Netherlands, in collaboration with biotechnology company Sanaria. It contains P. falciparum sporozoites that lack two genes the parasite needs in order to develop in the liver. Volunteers who were given the vaccine and then infected with malaria produced antibodies against CSP, along with immune system warriors called T cells (Sci. Transl. Med. 2020, DOI: 10.1126/scitranslmed.aaz5629).
Both vaccine trials involved a few dozen volunteers.
“Ultimately, these are promising results,” says Stefan H. I.Kappe, a malaria researcher at Seattle Children’s Research Institute, who was not involved in the trials and is developing a different genetically-attenuated sporozoite vaccine (Sci. Transl. Med. 2017, DOI: 10.1126/scitranslmed.aad9099). “I think we are at the beginning of developing a very potent attenuated whole-parasite vaccine.”




Join the conversation
Contact the reporter
Submit a Letter to the Editor for publication
Engage with us on Twitter