Advertisement
Grab your lab coat. Let's get started
Welcome!
Welcome!
Create an account below to get 6 C&EN articles per month, receive newsletters and more - all free.
It seems this is your first time logging in online. Please enter the following information to continue.
As an ACS member you automatically get access to this site. All we need is few more details to create your reading experience.
Not you? Sign in with a different account.
Not you? Sign in with a different account.
ERROR 1
ERROR 1
ERROR 2
ERROR 2
ERROR 2
ERROR 2
ERROR 2
Password and Confirm password must match.
If you have an ACS member number, please enter it here so we can link this account to your membership. (optional)
ERROR 2
ACS values your privacy. By submitting your information, you are gaining access to C&EN and subscribing to our weekly newsletter. We use the information you provide to make your reading experience better, and we will never sell your data to third party members.
Drug Delivery
Fatty acid-drug conjugate kills cancer cells in mice
The drug delivery system mimics dietary fatty acids and tricks tumor cells into taking up the conjugate
by Megha Satyanarayana
August 21, 2019

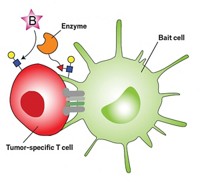
Chemists want to trick cancer cells into taking up drug molecules by attaching the payloads to fatty acids. These cells grow rapidly compared to normal cells and they recognize fatty acids as something they can quickly metabolize for energy, which means they could take up fatty acid-drug conjugates. But scientists say it has been challenging to develop a fatty acid-based drug-delivery system that cells will reliably take up. Now, a team of researchers have improved on this method by using a more realistic fatty-acid structure as the bait for cancer cells.
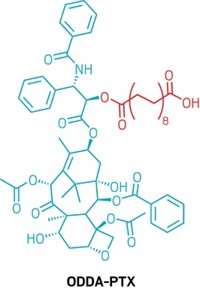
Developed by a team of researchers led by Nathan Gianneschi of Northwestern University, the drug delivery system, 1,18-octadecanedioic acid-paclitaxel, or ODDA-PTX, couples a long fatty acid chain with a molecule of paclitaxel, a chemotherapeutic drug that stops actively dividing tumor cells. They next mix the fatty acid-drug conjugate with albumin, a protein found in high concentration in the blood. Scientists have long studied it as a drug-delivery device because of its ability to hold other molecules in small pockets on its surface (J. Am. Chem. Soc. 2019, DOI: 10.1021/jacs.9b04272).
Making drugs more hydrophobic by coupling them to a fatty acid is a common drug-delivery process, Gianneschi says, but they’ve made some tweaks to improve both the circulation time of the drug conjugate and its uptake by tumor cells. For example, the scientists preserved the carboxylic acid at the end of the fatty-acid chain, which makes the conjugate look more like the fatty acids a cell would pick up to metabolize. Keeping the carboxylic acid also makes it more likely that albumin will stick the conjugate in its protein pockets. Gianneschi says that the more natural-looking design also fools dividing cancer cells into taking up the conjugate through active transport mechanisms, instead of letting it passively diffuse into the cells, which may lead to lower efficacy.
In unpublished experiments, the researchers tested ODDA-PTX against another fatty acid-based formulation of paclitaxel that doesn’t preserve the carboxylic acid and found that cancer cells actively take up ODDA-PTX more readily than the other formulation.
Once inside a tumor cell, two things can happen to ODDA-PTX to release the drug, Gianneschi says: Either the cell’s fat-metabolism machinery breaks down the fatty-acid chain until all that’s left is the active drug or routine hydrolysis cleaves the ester linkage between the fatty acid and the drug molecule.
To test the delivery system, Gianneschi’s team engrafted a human soft-tissue cancer into mice. After allowing the cancer to grow, the researchers tested ODDA-PTX on one group of the mice and a nanoparticle paclitaxel formulation on the market called Abraxane on another. They also tested paclitaxel in a delivery vehicle called Cremophor on a third group, and left a fourth group untreated.
After several weeks, the researchers found that the mice could tolerate ODDA-PTX at much higher doses than other formulations of paclitaxel, and at that high dose, tumors shrunk significantly and the mice lived longer than untreated animals. The researchers repeated these experiments in mice with human colorectal cancer and pancreatic cancer and saw similar results.
Cassandra Callmann, the lead researcher on the project, says that when they looked at metabolic markers of toxicity, the team found that they could give mice ODDA-PTX at doses almost 20 times that of Abraxane without observing signs of toxicity.
“I just like the simplicity,” says Martina Stenzel, a scientist at the University of New South Wales, who studies drug-delivery systems and who was not involved in the new work. She says that people in her field sometimes make drug delivery systems that are too complicated. “A lot of drug delivery vehicles are too much polymer, too much courier, and too little drug. You mix this drug with a fatty-acid derivative and it’s ready to go.”
The drug-delivery system could be used for other drugs, Gianneschi says. Callmann says the system might work to transport drugs to brain cancers, but they haven’t tested it yet. The scientists have founded a company called Vybyl Biopharma and are seeking funding to begin clinical trials of the delivery system.
CORRECTION
This story was updated on Aug. 15, 2019, to correct the spelling of Cassandra Callmann's name.



Join the conversation
Contact the reporter
Submit a Letter to the Editor for publication
Engage with us on Twitter