Advertisement
Grab your lab coat. Let's get started
Welcome!
Welcome!
Create an account below to get 6 C&EN articles per month, receive newsletters and more - all free.
It seems this is your first time logging in online. Please enter the following information to continue.
As an ACS member you automatically get access to this site. All we need is few more details to create your reading experience.
Not you? Sign in with a different account.
Not you? Sign in with a different account.
ERROR 1
ERROR 1
ERROR 2
ERROR 2
ERROR 2
ERROR 2
ERROR 2
Password and Confirm password must match.
If you have an ACS member number, please enter it here so we can link this account to your membership. (optional)
ERROR 2
ACS values your privacy. By submitting your information, you are gaining access to C&EN and subscribing to our weekly newsletter. We use the information you provide to make your reading experience better, and we will never sell your data to third party members.
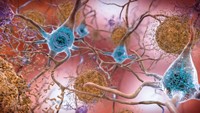
Neuroscience
Alzheimer’s drug candidate targeting bacterial protein has mixed results in trial
Cortexyme’s clinical trial of atuzaginstat failed, but the firm still sees hope for the drug
by Ryan Cross
October 28, 2021
| A version of this story appeared in
Volume 99, Issue 40
The small South San Francisco firm Cortexyme has an interesting theory about Alzheimer’s disease. The firm was founded based on evidence that a bacterium called Porphyromonas gingivalis—best known for causing gingivitis—infects brain cells, eats them from the inside out, and leaves a wake of destruction and inflammation that contributes to brain cell death and memory loss.

The remarkable hypothesis—that the devastating dementia whose cause and cure has long eluded neuroscientists is caused by a bacterial infection—demands remarkable evidence. Now, the company has its first results from a large clinical trial. It tested a drug candidate called atuzaginstat, which inhibits gingipains, protein-chomping enzymes made by P. gingivalis that have been found in the brains of people who died from Alzheimer’s disease.
By the broadest measure, the study was a failure. The Phase 2/3 trial looked at 643 people with mild to moderate Alzheimer’s disease. The drug did not significantly slow their cognitive or functional decline. Within a day of announcing the trial results, Cortexyme saw its stock fall by 75%.
But the company isn’t writing off its drug, which it contends could still be a boon to a large subset of people with Alzheimer’s disease. About one-third of the trial participants had P. gingivalis DNA in saliva samples taken at the beginning of the study. A portion of those individuals—the ones who got the highest dose of atuzaginstat—saw their cognitive decline slow by 57% compared to those who got a placebo pill.
In contrast, Aduhelm, the recently approved Alzheimer’s drug made by Biogen, slowed cognitive decline by about 22% in one clinical study and offered no statistically significant improvement in another. “I think that puts it in a little bit of context,” Cortexyme’s chief medical officer, Michael Detke, tells C&EN, although he admits that “comparing across studies is a little fraught.”
The company also says that people with lower levels of P. gingivalis DNA in their saliva after 24 weeks on the drug were more likely to have better outcomes on clinical tests designed to measure aspects of cognition like language and memory. Casey Lynch, CEO and cofounder of Cortexyme, says the results help reinforce her firm’s hypothesis about P. gingivalis.
“These are really intriguing results,” says Jeffrey Burns, codirector of the Kansas University Alzheimer’s Disease Center, who was not involved in the study. “These results will need to be replicated in a new study restricted to those who showed a potential benefit before wide use.”
The results were announced in a press release and a conference call with little supporting data. “It is certainly interesting,” says David S. Knopman, a clinical neurologist at the Mayo Clinic who was also not involved in the study. But since the results were announced in a press release, Knopman says he can’t “make any stronger statements about what the results mean.” Cortexyme says it will provide more details at the Clinical Trials on Alzheimer’s Disease Conference in Boston in November.
Lynch says her firm originally hoped that atuzaginstat could help most people with Alzheimer’s because, in one previous study, scientists found gingipains in nearly all brains of people who had died from the disease. But Cortexyme found that only a portion of Alzheimer’s patients tested positive for the infection. Even those who tested positive had varying responses to the drug, Lynch adds. The discrepancies are a mystery for now.
Knopman notes that while a high dose of atuzaginstat appeared to help slow cognitive decline, the drug didn’t significantly slow functional decline, as measured by a standard test of a person’s ability to perform activities like eating, walking, and using the bathroom independently. If the company were to redo the study in people who test positive for P. gingivalis and show that atuzaginstat can slow both cognitive and functional decline, “that would be very exciting,” he adds.
Cortexyme hasn’t specified its plans for the drug. “We are going to sit down with regulators and decide what is the most efficient path to get this drug closer to helping patients,” says Chris Lowe, the firm’s chief operating officer. That path might be conducting a new trial of the drug or requesting approval in a subset of people based on data from its current study.
Ruth Itzhaki, a professor emeritus of molecular neurobiology at the University of Manchester, says she was “impressed” by Cortexyme’s results in the group who tested positive for P. gingivalis. Itzhaki, who has studied the role of the herpes simplex type 1 virus in Alzheimer’s disease, hopes that Cortexyme’s trials will spur researchers to acknowledge the hypothesis that pathogens could cause or contribute to Alzheimer’s disease.
“Perhaps those in the Alzheimer’s disease field who have always opposed the infectious agent concept, despite their having no arguments against it, will now be able to understand it at last,” Itzhaki says.
Knopman would like to see more research on how P. gingivalis infections connect to traditional hallmarks of Alzheimer’s disease, such as amyloid plaques and tau tangles. “I am all in favor of pursuing novel approaches,” he says. “But I hope that they can eventually have the methodologic rigor and conceptual rigor to be acceptable to the scientific community in terms of showing benefit and understanding why that benefit occurs.”




Join the conversation
Contact the reporter
Submit a Letter to the Editor for publication
Engage with us on Twitter