Advertisement
Grab your lab coat. Let's get started
Welcome!
Welcome!
Create an account below to get 6 C&EN articles per month, receive newsletters and more - all free.
It seems this is your first time logging in online. Please enter the following information to continue.
As an ACS member you automatically get access to this site. All we need is few more details to create your reading experience.
Not you? Sign in with a different account.
Not you? Sign in with a different account.
ERROR 1
ERROR 1
ERROR 2
ERROR 2
ERROR 2
ERROR 2
ERROR 2
Password and Confirm password must match.
If you have an ACS member number, please enter it here so we can link this account to your membership. (optional)
ERROR 2
ACS values your privacy. By submitting your information, you are gaining access to C&EN and subscribing to our weekly newsletter. We use the information you provide to make your reading experience better, and we will never sell your data to third party members.
Vaccines
J&J shot is third COVID-19 vaccine authorized in US
Merck & Co. will help make the single-shot adenoviral vector vaccine, which protects against the emerging virus variants like B.1.351
by Ryan Cross
March 4, 2021
| A version of this story appeared in
Volume 99, Issue 8

The US Food and Drug Administration has authorized Johnson & Johnson’s COVID-19 vaccine for emergency use, making it the third such vaccine in the country. The announcement, made Feb. 27, came at a critical time—more than 500,000 people have died from COVID-19 in the US and new variants of SARS-CoV-2 threaten to make the pandemic worse.
Researchers closely following COVID-19 vaccine development tell C&EN they are not surprised the vaccine was authorized. J&J’s trial of nearly 44,000 people in multiple countries showed that a single shot was 77% effective at preventing severe and critical COVID-19 disease just 2 weeks after injection and 85% effective 4 weeks after injection. In preventing moderate or worse cases, it was 66% effective after 4 weeks. The FDA’s vaccine advisory committee voted unanimously in favor of authorizing the vaccine for people 18 and older.
“It was a very rigorously designed clinical trial,” says Lynda Coughlan, a virologist and vaccine scientist at the University of Maryland School of Medicine.
J&J was originally expected to deliver 37 million doses to the US government by the end of March, but now says it can deliver closer to 20 million, plus 80 million more doses by the end of June. That setback was offset by promising news that Merck & Co. would bolster manufacturing capacity for the vaccine. And on March 2, President Joe Biden said the US would have enough shots—including the previously authorized Pfizer-BioNTech and Moderna vaccines—for every adult in the US by the end of May, although getting the vaccines into people’s arms will take longer.
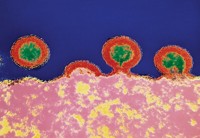
J&J’s shot is based on adenoviral vector vaccine technology, in which a genetically engineered cold virus is used to deliver the DNA for the SARS-CoV-2 spike protein into human cells. The Pfizer-BioNTech and Moderna vaccines, in contrast, use messenger RNA (mRNA) inside lipid nanoparticles to deliver genetic instructions for the spike protein into human cells.
The mRNA vaccines were both about 95% effective at preventing COVID-19 in clinical trials, but scientists warn against comparing the different vaccines head-to-head. “I wouldn’t put much emphasis on it at all,” says Tony Moody, an immunologist at the Duke Human Vaccine Institute. “Having yet another vaccine out there will allow more people to get vaccinated. I think that’s probably the more important thing.”
The clinical trials for the vaccines were conducted in different places, with different populations, and at different times, Coughlan notes. “I am not a fan of comparing the percentages. I don’t think it is helpful.” Such comparisons, she notes, often overlook the distinction between preventing any cases of COVID-19, including mild ones, and preventing the severe and critical cases that can lead to hospitalization and death.
But there are some differences that researchers think are worth emphasizing. While the mRNA vaccines require two shots, administered 3 or 4 weeks apart, J&J’s vaccine was authorized as a single shot. And while the mRNA vaccines have to be shipped and stored in freezers, J&J’s vaccine can be stored for up to 3 months in regular refrigerator temperatures of 2–8°C.
“You can’t overstate how much easier the cold chain issues are with adenoviral vector vaccines compared to mRNA vaccines,” says David Curiel, director of the Biologic Therapeutics Center at the Washington University School of Medicine in St. Louis. “So it is a positive addition to the vaccine armamentarium that is being rolled out.”
The J&J vaccine will also be cheaper, Coughlan notes. That plus its less stringent temperature requirements could make the vaccine “a complete game changer” for countries that don’t have plans to purchase the mRNA vaccines, she says.
In February, a preliminary report of J&J’s trial suggested that the vaccine was less effective in South Africa. A new variant of the virus known as B.1.351 was first identified in South Africa in December and circulated widely there during J&J’s study. That variant, plus other variants that share similar mutations in the SARS-CoV-2 spike protein, is now spreading in the US, stoking fears that COVID-19 vaccines designed in early 2020 won’t be good enough.
More detailed data that J&J presented to the FDA suggests that the vaccine will still protect against B.1.351. The shot was about 82% effective at preventing severe or critical COVID-19 in South Africa, compared to being about 86% effective in the US.
“They had very good efficacy, even in the face of that variant, and that is quite reassuring,” Coughlan says. The vaccine was 64% effective at preventing moderate to critical cases of COVID-19 in South Africa, compared to 72% in the US, meaning that the shot still meets the FDA’s cutoff of 50% effectiveness.
Some lab studies suggest that the antibody response induced by the mRNA vaccines is not as good at protecting against new variants like B.1.351, but scientists caution against overinterpreting these results. “The variants are only partially resistant,” Moody says. “It is not an all-or-none phenomenon.” The variants may reduce the effectiveness of the vaccines a bit, but turning a severe case of COVID-19 into a mild case is still a big benefit, he adds. “If anything, the variants just emphasize why people need to get vaccinated.”
There’s another nuance missing from concerns about the variants. Studies on variants often focus on whether neutralizing antibodies induced by the vaccines can bind to the SARS-CoV-2 spike protein and prevent it from infecting cells. Those neutralizing antibodies are important, but they are not the only part of the immune system that vaccines rev up. T cells are important too, Coughlan says. “Although they don’t prevent infection, they can minimize the severity of symptoms and reduce viral shedding, meaning that they could have an impact on transmission.” The adenoviral vector and mRNA vaccines both induced T-cell responses in clinical trials.
A booster shot might make the vaccines better at protecting against B.1.351 and other variants, and J&J is running a clinical trial to see if giving people a second shot of its vaccine would provide better results. Small trials testing a second booster shot—a third shot in total—of the Moderna and Pfizer-BioNTech vaccines are underway as well. And all four companies are working on new constructs of their vaccines based on variants such as B.1.351.
Merck’s role in helping to manufacture J&J’s vaccine will aid in getting the vaccine into more arms more quickly. “It is unusual and exciting” to see the competitors collaborate, Moody says. Merck abandoned two experimental COVID-19 vaccines after disappointing Phase 1 clinical studies. “So this is a good move from a Merck public relations perspective, but it also keeps them in the game,” Moody adds.
Merck is familiar with manufacturing adenoviral vector vaccines because the firm had run large clinical trials of an experimental HIV vaccine based on the technology in the mid-2000s. Unlike the mRNA vaccines, which are chemically synthesized and rely on ingredients that are in short supply, adenoviral vector vaccines are grown in cells, a vaccine-manufacturing technique that is more widely used and readily shared between companies. “I was kind of surprised that they hadn’t got involved up until this point, but it is great news,” Coughlan says.
Scientists are excited to see the vaccines get to more people. On March 2, the US Centers for Disease Control and Prevention reported that over 100 million doses of COVID-19 vaccines have been delivered throughout the US. More than 51 million individuals have gotten at least one of their two shots of the mRNA vaccines. Still, vaccine scientists urge the public to not drop its guard against the virus too quickly.
“Vaccination is not a substitute for precaution, it is an adjunct to precaution,” Moody says. “The fastest way to get back to normal is to get vaccinated, and continue to wear your mask and social distance until we can smack this thing down.”




Join the conversation
Contact the reporter
Submit a Letter to the Editor for publication
Engage with us on Twitter