Advertisement
Grab your lab coat. Let's get started
Welcome!
Welcome!
Create an account below to get 6 C&EN articles per month, receive newsletters and more - all free.
It seems this is your first time logging in online. Please enter the following information to continue.
As an ACS member you automatically get access to this site. All we need is few more details to create your reading experience.
Not you? Sign in with a different account.
Not you? Sign in with a different account.
ERROR 1
ERROR 1
ERROR 2
ERROR 2
ERROR 2
ERROR 2
ERROR 2
Password and Confirm password must match.
If you have an ACS member number, please enter it here so we can link this account to your membership. (optional)
ERROR 2
ACS values your privacy. By submitting your information, you are gaining access to C&EN and subscribing to our weekly newsletter. We use the information you provide to make your reading experience better, and we will never sell your data to third party members.
Lab Safety
What is an allergy sensitizer, and how does a chemical become one?
One researcher now risks death if she enters her former lab building
by Benjamin Plackett, special to C&EN
May 1, 2020
| A version of this story appeared in
Volume 98, Issue 18

Kate McKnelly expects to finish up her PhD this summer, but she isn’t allowed to set foot in her laboratory at the University of California, Irvine. That’s because she is effectively allergic to the building.
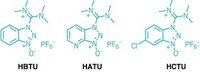
She had been handling peptide coupling agents for years when in 2018 she started to develop a severe and potentially life-threatening reaction to three of them: HATU, HBTU, and HCTU. While HATU and HBTU were already known to cause allergic reactions, McKnelly’s case appears to be the first to involve HCTU as an allergy sensitizer.
“If you look at a chemical label and it says ‘Flammable,’ then you know to be really careful. Or if it’s a carcinogen, then you know it can cause cancer. You have a good grasp on what those words mean,” McKnelly says. “Sensitizer is a more nebulous term.”
Sensitizers are chemicals with the potential to become allergens. It’s hard to predict which chemicals will be sensitizers, who is likely to be vulnerable to them, and how much exposure will induce a reaction. Consequently, working safely in a lab means handling known sensitizers and chemically similar compounds cautiously to minimize exposure.
Various parts of the immune system are constantly on the prowl for substances they don’t recognize. That’s how viral or bacterial infections are detected. An allergic reaction essentially involves duping the body’s immune system to push it into overdrive.
The molecular weight of an individual chemical compound is typically too small to elicit an immune reaction. “So they need to bind with a so-called carrier protein to create an allergen and therefore a response,” explains Susan Tarlo, a respiratory physician and professor of medicine at the University of Toronto.
To become a sensitizer, a chemical binds with a human protein in a way that slightly alters the protein’s structure. That altered structure causes the immune system to perceive it as a foreign substance, triggering production of an antibody to recognize the modified protein, says Robin Bon, a professor of chemical biology at the University of Leeds. Any protein can be a carrier protein if binding of a small molecule causes the immune system to identify it as foreign.
After the immune system starts making the antibody, it hangs out in the blood, waiting to see if that particular chemical-protein combination appears again. When that happens, the antibody activates the immune system to release histamines and other molecules and enzymes that cause an inflammatory response, Bon says.
The severity of symptoms can range from a mild runny nose or itchy skin to full-blown anaphylaxis, as was the case with McKnelly. Symptoms of anaphylaxis include trouble breathing, hives, vomiting, and low blood pressure. Anaphylaxis can be fatal.
Two kinds of chemical sensitizers exist: those that cause symptoms in the respiratory system and those that affect the skin. “By far, skin allergies are the more common of the two,” says David Basketter, a scientist at Dabmeb Consultancy whose research focuses on chemical allergies. However, respiratory allergens tend to generate more severe symptoms. “There’s also a small subset that are both skin and respiratory sensitizers, such as phthalic anhydride,” Basketter adds.
While scientists believe chemical sensitization is uncommon, “there are many chemicals that can cause sensitization in certain people,” Bon says. “Definitely not just peptide coupling agents.”
Certain metals, such as nickel; pharmaceutical ingredients, including some antibiotics; and cosmetic components—in particular, dyes and bleaches—are known to act as chemical sensitizers for some people. What they all have in common, Bon says, is their ability to interact with human proteins to change their chemical structures.
But it’s hard to predict which chemicals, other than those that scientists already know about, are likely candidates to provoke an allergic response. Some key classes of respiratory sensitizers include acid anhydrides, diisocyanates, some platinum salts, a few amines, and certain aldehydes—notably glutaraldehyde, Basketter says. “But remember that in each of these groups, lots of members do not appear to cause respiratory allergy,” he says.
Some researchers think certain chemical properties make a substance more likely to cause problems—highly reactive agents are, by their very nature, more likely to be able to bind to a human protein. But even that’s “rather speculative,” Tarlo cautions.
“Unfortunately, it’s mostly theory because there are very few chemicals with which we can show a very clear allergic response,” she says. That’s because the immune system produces a specific antibody for each allergen. The best way to confirm the cause of an allergic reaction is to find the allergen’s distinct antibody in a blood test. But if scientists don’t know what the antibody looks like, then they’re just stabbing in the dark. That can be a particular challenge if someone develops allergies in a lab that may handle a plethora of different substances.
McKnelly says she first started to suspect she was becoming allergic to the peptide coupling agents when she experienced a runny nose and sneezing after she spilled some HCTU. When the allergy later became more severe, she and her allergist were able to determine the cause through skin prick testing because they already had a good idea of which chemicals were causing the reaction .
All three coupling agents caused her to break out in large hives when she was pricked. Her allergist, who performed the same tests on himself as a control subject, showed no reaction. That’s a fairly convincing diagnosis, but it required McKnelly to have a clear suspicion of what was causing the symptoms in the first place—a luxury not every clinician has.
McKnelly first started to work with the three peptide coupling agents when she was doing her master’s degree at the University of Leeds in 2014 in the lab of chemistry professor Andrew Wilson. It’s hard to pinpoint exactly when she started to become sensitized to these chemicals.
“There is a latency period,” Tarlo says. “It takes time to form antibodies, so you wouldn’t expect someone to have an allergic response the first day they’re exposed. It could be anywhere from 10 days to many years,” but typically symptoms appear in the first 2 years of exposure.
However, McKnelly’s exposure to the sensitizers was probably lower during her studies in Leeds because her lab there followed more stringent safety procedures than her lab at UCI. For example, even though HCTU wasn’t yet proven to be a sensitizer, awareness of safety protocols for HATU and HBTU encouraged cautious behavior, Wilson says.
“Any peptide coupling agent, in my view, can become a sensitizer because of the way they work and what they do,” Wilson says.
So, he required people working in his lab to weigh the chemicals in a ventilated fume hood in addition to wearing the usual gloves and lab coats. Additionally, anyone regularly using HATU or HBTU was referred to the university’s occupational health department for monitoring. After he learned of McKnelly’s allergies, Wilson added HCTU to the list of chemicals that require health monitoring. He has also updated his lab’s risk assessment paperwork with new links to relevant literature and reemphasized that any agent can potentially cause sensitization.
The situation was different in Irvine, where McKnelly didn’t use a ventilated hood. “I was kind of annoyed at myself because I had come to the university from a lab that handled the chemicals well,” she says. “Maybe I should have spoken up to say that.”
But she says her lab in California had been using the peptide coupling agents outside hoods since the early 2000s, and she is the only person to have become sensitized during that time. Since McKnelly’s sensitization, the lab has instituted new procedures for handling sensitizers (J. Org. Chem. 2019, DOI: 10.1021/acs.joc.9b03280). According to a literature search conducted by McKnelly and two colleagues, only nine cases of sensitization from HATU and HBTU have been published since 2003, and McKnelly’s is the first case reported for HCTU.
Other unreported case studies may exist, Basketter says. “One of the issues is that publication is not high on most clinicians’ to-do lists. Their concern is treating patients,” he says. “Accordingly, unless a case or, better still, a group of cases, is really interesting, they may well not bother.”

Benjamin Plackett is a freelance writer based in the UK. A version of this story first appeared in ACS Chemical Health and Safety: cenm.ag/chemicalallergies.



Join the conversation
Contact the reporter
Submit a Letter to the Editor for publication
Engage with us on Twitter