Advertisement
Grab your lab coat. Let's get started
Welcome!
Welcome!
Create an account below to get 6 C&EN articles per month, receive newsletters and more - all free.
It seems this is your first time logging in online. Please enter the following information to continue.
As an ACS member you automatically get access to this site. All we need is few more details to create your reading experience.
Not you? Sign in with a different account.
Not you? Sign in with a different account.
ERROR 1
ERROR 1
ERROR 2
ERROR 2
ERROR 2
ERROR 2
ERROR 2
Password and Confirm password must match.
If you have an ACS member number, please enter it here so we can link this account to your membership. (optional)
ERROR 2
ACS values your privacy. By submitting your information, you are gaining access to C&EN and subscribing to our weekly newsletter. We use the information you provide to make your reading experience better, and we will never sell your data to third party members.
Medicinal Chemistry
This chili pepper compound will self-destruct
To relieve itch and pain without undesirable side effects, chemists put a kill switch on capsaicin
by Deirdre Lockwood, special to C&EN
June 6, 2018

Capsaicin, the compound that gives chili peppers their heat, is added to some medical creams because of its ability to ease pain and itch. But along with this relief, capsaicin and some of its derivatives can deliver troubling side effects. Now researchers have modified a derivative of capsaicin so that it is inactivated within hours by enzymes in the skin, averting some of these side effects while demonstrating pain and itch relief in mice (J. Med. Chem. 2018, DOI: 10.1021/acs.jmedchem.8b00109).
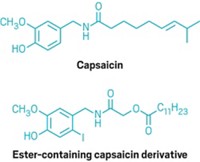
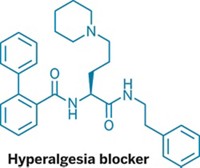
Capsaicin soothes pain and itch by propping open an ion channel called TRPV1 in cells. But not surprisingly, given its spicy reputation, it also burns. Related derivatives made in part by replacing hydrogen with iodine in one spot in the capsaicin molecule also help with pain and itch via a different mechanism—by blocking the same channel. These versions don’t burn but can disrupt temperature regulation in the body, leading to fever spikes called hyperthermia. And both types of these TRPV1-acting compounds can foster skin tumor formation in mice when combined with a tumor promoter, like sunlight. Sun exposure is a special concern for topical application, particularly because capsaicin is lipophilic and stays in the skin for a long time.
To overcome these problems, Asia Fernandez-Carvajal of Miguel Hernández University, Tracey Pirali of the University of Eastern Piedmont, and their colleagues made a variety of capsaicin derivatives with a built-in self-destruct switch, with the goal of relieving pain and itch in the short term while avoiding some of these side effects. The switch took the form of an ester bond in the tail of the compounds, which they introduced using the Passerini reaction, a type of reaction seldom used in medicinal chemistry because it makes molecules more degradable in the body. This bond is hydrolyzed by esterase enzymes in skin into two metabolites that the body easily eliminates. This so-called “soft drug” approach has been used in other medicines, such as the beta blocker esmolol, to control their elimination in the body.
The researchers first tested the compounds for activity on the TRPV1 channel in human neuroblastoma cells, and then assayed the most potent candidates in human skin cells to determine those that were significantly hydrolyzed. Finally, they tested in mice a molecule that performed well in both tests. They injected the paws of one group of mice with an emulsion containing heat-killed bacteria—which causes inflammation that makes the paws more sensitive to heat and touch—and two other groups with histamine and chloroquine, respectively, to stimulate itch. Then they injected the capsaicin derivative or a control substance into the paws of the mice. The molecule reduced sensitivity to heat and touch in the first set of mice and to itch in the other two sets, without producing hyperthermia. The effects lasted up to 90 minutes after injection; however, study coauthor Antonio Ferrer-Montiel of Miguel Hernández University says that relief may last longer with a topical cream because the compound would need to pass through the epidermis to the dermis before encountering esterases that could degrade it.
Advertisement
Baskaran Thyagarajan, a pharmaceutical scientist at the University of Wyoming who studies this family of channels, calls the study convincing. He says that the molecule’s biological availability, pharmacokinetics, and pharmacodynamics must be tested, which the researchers plan to do next. He adds that the study opens up a new direction for developing modulators of the TRPV1 channel to potentially treat other conditions thought to be linked to TRPV1 activity, such as type 2 diabetes and hypertension.



Join the conversation
Contact the reporter
Submit a Letter to the Editor for publication
Engage with us on Twitter