Advertisement
Grab your lab coat. Let's get started
Welcome!
Welcome!
Create an account below to get 6 C&EN articles per month, receive newsletters and more - all free.
It seems this is your first time logging in online. Please enter the following information to continue.
As an ACS member you automatically get access to this site. All we need is few more details to create your reading experience.
Not you? Sign in with a different account.
Not you? Sign in with a different account.
ERROR 1
ERROR 1
ERROR 2
ERROR 2
ERROR 2
ERROR 2
ERROR 2
Password and Confirm password must match.
If you have an ACS member number, please enter it here so we can link this account to your membership. (optional)
ERROR 2
ACS values your privacy. By submitting your information, you are gaining access to C&EN and subscribing to our weekly newsletter. We use the information you provide to make your reading experience better, and we will never sell your data to third party members.
Biochemistry
Engineered universal blood made possible by bacterial enzymes
The blood type converting process could help ease the demand for type O blood
by Sarah Braner
May 2, 2024
| A version of this story appeared in
Volume 102, Issue 14

Bacterial enzymes may help increase the supply of universal blood.
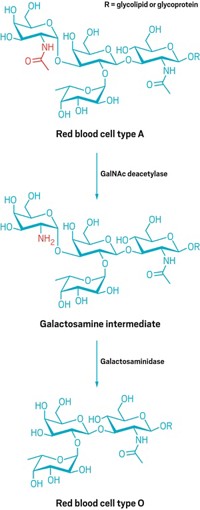
There is an outsize demand for type O blood, specifically because it includes red blood cells that can be transfused into anyone without the risk of the recipient’s immune system attacking those cells. This is because types A and B blood cells have characteristic sugar molecules attached to the H antigen, while type O blood cells simply present the H antigen. This feature makes type O blood the most valuable in an emergency when a patient needs a transfusion but there’s no time to determine their blood type. This demand means that type O blood is the first to run out during a blood shortage, but a solution may be on the way.
Labs from Lund University and the Technical University of Denmark led by Martin Olsson and Maher Abou Hachem, respectively, took enzymes from a bacterium called Akkermansia muciniphila, which degrades mucin in the human gut. The mucin that A. muciniphila targets has sugar molecules on its surface, similar to those on type A and B red blood cells, which make the enzymes this bacterium produces an attractive prospect for blood conversion. The enzymes were able to degrade the sugars on the surface of blood cells and convert type A and B blood to universal O blood. (Nat. Microbiol. 2024, DOI 10.1038/s41564-024-01663-4)
As early as 1982, researchers used an enzyme called α-galactosidase from green coffee beans to remove the characteristic sugar from the surface of type B blood cells and convert them to type O (JAMA, J. Am. Med. Assoc. 1982, DOI 10.1001/jama.1982.03320260004002). While this suggested that enzymatic blood conversion is possible, not all the blood cells created by that process were compatible with recipient plasma. The cause for that wasn’t clear.
The new research suggests that enzymes used in the past were likely not accounting for extended forms of the surface antigens found on type A and B red blood cells.
“We knew they were there,” Olsson says. “But everyone thought they were harmless.” The researchers now believe that these extensions probably do matter and that the enzymes from the gut bacteria identified by this group can target these extensions. Up to 98% of the engineered O cells that were made from type B passed the compatibility test, and almost 50% of the cells made from type A passed. This is likely because type A cells are a more complicated target, with three extended forms, while type B cells have only one known extended form.
These enzymes have another critical advantage over the coffee bean enzyme used previously: they’re much more efficient, and as a result, you need fewer of them to convert the blood cells. This saves enzymes and reduces the risk of possible off-target effects.
That risk may not be completely gone, however. “We don’t know what else those enzymes they are adding might be doing. Because there may be other important sugars on the surface of the red blood cell that are being removed that, in another context, could cause issues,” says Stephen Withers, a researcher who is on the board of directors for Avivo, a company that’s developing more universally accepted blood and organs. He was not involved with the study and published a separate method for converting type A blood in 2019.
Hachem mentioned that avoiding unintended effects is important and an issue the team will continue to study. The researchers may also need to identify additional enzymes to convert blood antigen extensions that have not yet been discovered.


Join the conversation
Contact the reporter
Submit a Letter to the Editor for publication
Engage with us on Twitter