Advertisement
Grab your lab coat. Let's get started
Welcome!
Welcome!
Create an account below to get 6 C&EN articles per month, receive newsletters and more - all free.
It seems this is your first time logging in online. Please enter the following information to continue.
As an ACS member you automatically get access to this site. All we need is few more details to create your reading experience.
Not you? Sign in with a different account.
Not you? Sign in with a different account.
ERROR 1
ERROR 1
ERROR 2
ERROR 2
ERROR 2
ERROR 2
ERROR 2
Password and Confirm password must match.
If you have an ACS member number, please enter it here so we can link this account to your membership. (optional)
ERROR 2
ACS values your privacy. By submitting your information, you are gaining access to C&EN and subscribing to our weekly newsletter. We use the information you provide to make your reading experience better, and we will never sell your data to third party members.
Analytical Chemistry
Nanoconjugates Trigger Cancer Cell Suicide
Bioengineering: New cancer treatment strategy could avoid the side effects of conventional immunotherapy by using matching nanomaterials that meet up on the surface of cancer cells
by Leigh Krietsch Boerner
January 7, 2014

Drugs designed to treat certain cancers, such as non-Hodgkin’s lymphoma, recruit the body’s own immune system to attack the rogue cells. But less than half of all patients respond to such immunotherapies, and the drugs can have severe side effects. Now, researchers introduce a new type of therapy that could potentially avoid these problems. They designed a pair of nanomaterials that attach to each other on the surface of cancer cells, tricking the cells into killing themselves (ACS Nano 2013, DOI: 10.1021/nn4053827).
The researchers, led by Jindřich Kopeček, a biomedical polymer chemist from the University of Utah, borrowed the concept from the field of biomaterials, where scientists often design individual material components that have to pair up to do a job. Kopeček’s team made two materials that would attack non-Hodgkin’s lymphoma cells without the use of conventional drugs. The components would only be active when used together, and in a particular order.
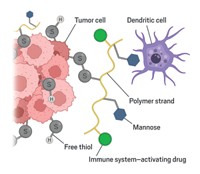
The treatment system targets the B-lymphocyte antigen CD20, a protein that decorates the surface of immune cells called B cells. Non-Hodgkin’s lymphoma often originates in these B cells, so the treatment attacks the cancer cells as they grow. The researchers synthesized two nanomaterials designed to pair with each other in such a way as to trigger apoptosis, or programmed cell death, in those cells. The first nanomaterial consists of a CD20 antibody known as Fab′ attached to a nucleic-acid-like oligomer called MORF1. When this material is added to B cells, the antibody attaches to CD20 proteins, leaving the MORF1 oligomers dangling from the surface of the cells.
The second nanomaterial consists of a linear polymer called HMPA decorated with multiple copies of an oligomer complementary to MORF1 called MORF2. When this material is added to B cells, the MORF2s bind to MORF1s labeling CD20s on the cell surfaces. Because the MORF2s are all on a single polymer chain, the individual CD20s are brought into close proximity with each other and begin to crosslink with their neighbors. The crosslinking of the CD20 proteins on the cell surface opens calcium channels inside the cell, which triggers apoptosis.
To test the therapy, the team first put human non-Hodgkin’s lymphoma cells in mice, which seeds tumor growth in the brain and spinal column. Next they injected the mice with the nanoconjugate containing the Fab′ fragment and MORF1. After an hour, they injected the piece containing MORF2 and HPMA. After three rounds of this treatment, all the mice receiving the nanomaterial pair survived for 125 days and were free of tumors. Mice that did not receive the treatment only lived around 33 days after the tumor cell injection, and magnetic resonance imaging showed evidence of tumors in the spine, lung, brain, and liver after their deaths.
“It’s a totally new paradigm in drug delivery,” Kopeček says. “We have created a new system where low molecular-weight drugs are not needed.” In addition, each part of the treatment system is inactive and harmless if given individually in the animal model, he says. And, in a cell-based test of the method, the team found that the nanoconjugates caused cell death only when given in the proper order.
This highly innovative strategy can potentially improve the targeting efficiency and reduce side effects of cancer treatment, says Kam W. Leong, a biomedical engineer at Duke University. However, since it’s unclear if these nanoconjugates can be used on other cell types, he’s not sure if this method can replace other currently used drug delivery procedures for most cancers.
Kopeček and his research group next plan to optimize the therapy and get it into clinical trials, which they think may happen in as few as five years. They also think that they can translate the method to other cancers by using similar antigens, such as those linked to prostate cancer.




Join the conversation
Contact the reporter
Submit a Letter to the Editor for publication
Engage with us on Twitter