Advertisement
Grab your lab coat. Let's get started
Welcome!
Welcome!
Create an account below to get 6 C&EN articles per month, receive newsletters and more - all free.
It seems this is your first time logging in online. Please enter the following information to continue.
As an ACS member you automatically get access to this site. All we need is few more details to create your reading experience.
Not you? Sign in with a different account.
Not you? Sign in with a different account.
ERROR 1
ERROR 1
ERROR 2
ERROR 2
ERROR 2
ERROR 2
ERROR 2
Password and Confirm password must match.
If you have an ACS member number, please enter it here so we can link this account to your membership. (optional)
ERROR 2
ACS values your privacy. By submitting your information, you are gaining access to C&EN and subscribing to our weekly newsletter. We use the information you provide to make your reading experience better, and we will never sell your data to third party members.
Materials
Designer coatings fight infections and help bones heal
Multilayer thin films could fight costly and difficult-to-treat prosthetic infections
by Prachi Patel
March 11, 2016

An ultrathin coating for prosthetics fights bacterial infections and speeds up bone healing around implants tested in rats (ACS Nano 2016, DOI: 10.1021/acsnano.6b00087). After delivering a high-dose burst of antibiotics in the first few days, the coating continues to release the drug for weeks along with a protein that spurs bone growth. The goal is to cut the rate of prosthetic infections, which takes lives and could cost the healthcare system at least $1.6 billion by 2020 as increasingly more people get artificial joints.
The number of people over 45 years of age who get hip replacements has more than doubled from 2000 to 2010, from about 140,000 to more than 310,000. About 5% of patients with hip implants develop bacterial infections, with the rate much higher for shoulder implants. Treatment involves two surgeries: one to remove the infected implant and deliver antibiotic-releasing beads at the site, and another a few weeks later to remove the spent beads and put in a new implant.
“Our implant coating would eliminate the need for this two-stage process and reduce the cost of hospitalization,” says Paula T. Hammond, a chemical engineer at Massachusetts Institute of Technology.
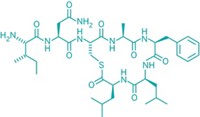
Hammond and her colleagues make the coating using a process called layer-by-layer assembly, which involves depositing alternating layers of oppositely charged molecules onto a surface, forming multilayered films nanometers to micrometers thick. They have used the technique to make glues for bone implants and bandages that release multiple drugs for wound healing.
The new 0.5- to 2-µm-thick coating has two parts: a top layer that releases the antibiotic gentamicin and a bottom layer that releases BMP-2, a protein that triggers bone growth. Each layer consists of a polymer base topped with two poly(acryclic acid) films, which biodegrade to release the therapeutic molecules sandwiched in the middle. By changing the types of polymers used and the number of repeated layers, the researchers can customize how much drug is released and how fast.
Releasing tailored quantities of two different molecules at appropriate time scales makes the coating especially effective, Hammond says. Another key advantage is that it could be easily deposited on implants of any material, size, and shape.
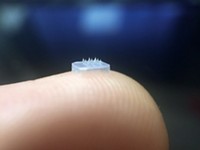
The researchers tested the release profile of the molecules by immersing a 1.3-mm-wide, 4-mm-long coated implant in saline buffer solution. They measured a 60-µg burst of antibiotic on the first day followed by 1 µg released daily over 40 days. Meanwhile, 110 ng of the growth factor was released per day for the first six days followed by about 13 ng per day for the remaining time.
Then the researchers surgically placed uncoated and coated polymer implants in the shinbone of rats in which they had induced bacterial infection. After three weeks, untreated implants had bacterial films growing on them while the coated implants were clean. After eight weeks, animals who received untreated implants had severe infection and bone damage. Over the same time period, animals with coated implants had healthy bone tissue growing on and around them, and their shinbones were 15 times stronger than in untreated animals.
Antibiotic coatings for implants is not a new concept, says Julie A. Champion, a biomaterials engineer at Georgia Tech. But controlled release of antibiotics with bone growth factors makes the approach valuable. “These two molecules have a synergistic effect because infection prevents bone regrowth, and bone regrowth prevents infection,” she says. The simple fabrication process and known materials should make the coating practical, she says, but the researchers will first need to show safety and efficacy in larger animals.



Join the conversation
Contact the reporter
Submit a Letter to the Editor for publication
Engage with us on Twitter