Advertisement
Grab your lab coat. Let's get started
Welcome!
Welcome!
Create an account below to get 6 C&EN articles per month, receive newsletters and more - all free.
It seems this is your first time logging in online. Please enter the following information to continue.
As an ACS member you automatically get access to this site. All we need is few more details to create your reading experience.
Not you? Sign in with a different account.
Not you? Sign in with a different account.
ERROR 1
ERROR 1
ERROR 2
ERROR 2
ERROR 2
ERROR 2
ERROR 2
Password and Confirm password must match.
If you have an ACS member number, please enter it here so we can link this account to your membership. (optional)
ERROR 2
ACS values your privacy. By submitting your information, you are gaining access to C&EN and subscribing to our weekly newsletter. We use the information you provide to make your reading experience better, and we will never sell your data to third party members.
Infectious disease
Different paths, same goal: A new study shows how COVID-19 variants thrived
Changes in certain nonspike proteins helped SARS-CoV-2 variants get past the body’s first line of defense against invaders
by Priyanka Runwal
October 5, 2023
| A version of this story appeared in
Volume 101, Issue 33

To protect people from acquiring severe COVID-19 infections, researchers have typically targeted SARS-CoV-2’s spike protein. “That’s important,” says Nevan Krogan, a molecular biologist at the University of California, San Francisco. “But there are 28 other genes on the virus.”
These protein-coding genes acquired mutations as the virus spread, giving rise to variants. In a recent study, Krogan and his colleagues found that SARS-COV-2 variants developed mutations linked to specific proteins in the nonspike region that helped the virus multiply and spread rapidly (Cell 2023, DOI: 10.1016/j.cell.2023.08.026). Some variants also regulated the expression of certain other nonspike proteins to reach the same end goal to outsmart the body’s first line of defense, the innate immune system.
“How the different variants get there follows different mutational trajectories,” Krogan says, “but the end result is the same.”
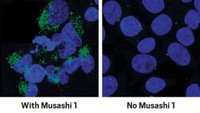
A nonspike protein called ORF9b, for example, was involved in allowing the Alpha, Beta, Gamma, and Delta variants of the SARS-CoV-2 virus to evade the innate immune system. Although the original Omicron variant strain, BA.1,was less effective at suppressing this defense, its subvariants, including BA.4 and BA.5, succeeded by producing higher levels of another protein, called ORF6.
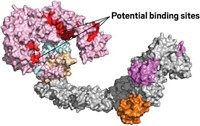
The research team is now trying to develop drugs that would reduce the levels of nonspike protein expression or block these proteins from binding to the ones in host cells, says coauthor Adolfo García-Sastre, a molecular biologist at the Icahn School of Medicine at Mount Sinai. The drugs could help slow down or end an existing COVID-19 infection. But in the long run, a “cocktail therapy” that acts on multiple viral targets will be needed, Krogan adds.
For now, Matthew Frieman, a virologist at the University of Maryland who was not involved in the research, would like to see if the observations Krogan and his colleagues made in human lung cells hold up when animals are subjected to similar changes in key nonspike proteins. “All these interactions have to be validated in multiple systems,” he says.



Join the conversation
Contact the reporter
Submit a Letter to the Editor for publication
Engage with us on Twitter