Advertisement
Grab your lab coat. Let's get started
Welcome!
Welcome!
Create an account below to get 6 C&EN articles per month, receive newsletters and more - all free.
It seems this is your first time logging in online. Please enter the following information to continue.
As an ACS member you automatically get access to this site. All we need is few more details to create your reading experience.
Not you? Sign in with a different account.
Not you? Sign in with a different account.
ERROR 1
ERROR 1
ERROR 2
ERROR 2
ERROR 2
ERROR 2
ERROR 2
Password and Confirm password must match.
If you have an ACS member number, please enter it here so we can link this account to your membership. (optional)
ERROR 2
ACS values your privacy. By submitting your information, you are gaining access to C&EN and subscribing to our weekly newsletter. We use the information you provide to make your reading experience better, and we will never sell your data to third party members.
Gene Editing
From ‘science fiction’ to ‘just hard’: Mitochondrial DNA editing inches closer to reality
Compared with altering the nuclear genome, mitochondrial gene editing has different hurdles that drug developers need to navigate
by Shi En Kim
May 26, 2023
| A version of this story appeared in
Volume 101, Issue 17

Over a billion years ago, a single-celled archaean engulfed an overachieving bacterium. The bacterium didn’t perish but instead struck an agreement with its host. For shelter, the bacterium would pay rent by doing what it did best—churn out energy molecules to power both itself and the host cell.
This pivotal event in Earth’s history, according to the endosymbiosis theory, allowed the nested cells to harvest energy from the environment like never before, thus starting the march toward complex life. From such simple prokaryotic life forms came nucleus-toting eukaryotes and then their multicellular counterparts, eventually giving rise to the organismic richness across the planet today. With a few exceptions, most modern eukaryotic cells harbor these once-free-roaming bacteria. We call them mitochondria.
Over the eons, mitochondria coevolved with their hosts as organelles, but the former bacteria never fully jettisoned their genes. In a last-ditch streak of independence, mitochondria retained 37 genes to code for 13 proteins, leaving the remaining 99% of the proteins it needs to the nuclear genome. But where there are genes, there is replication—and errors are bound to arise. Mutations in mitochondria- associated genes lead to mitochondrial diseases. These multisystemic disorders can impact any organ, though those with the highest energy demands, such as the brain and heart, tend to be the most affected.
Mitochondrial diseases affect 1 in every 4,300–6,700 people, according to independent studies on hospital diagnoses in different countries. The disease symptoms and severity can be varied, even among people with the same mutation. In 2018, a survey revealed that people see an average of eight clinicians before receiving an accurate diagnosis for mitochondria-related conditions. To date, no cures exist, only symptom management.
“There’s a big unmet need to treat mitochondrial diseases,” says Michio Hirano, a Columbia University neurologist who was one of the authors of the 2018 survey.
But where there are genetic errors, there’s also an opportunity to correct them. Enter mitochondrial gene editing, which aims to tackle the roots of mitochondrial diseases once and for all. While the technology is still years away from treating patients, academic and industry interest in the concept and its clinical potential is growing.
A different beast
Compared with gene editing in the nucleus, gene editing in mitochondria is a different beast. Hitting their 37 genes is tricky. These genes are walled off from the rest of the cell by the mitochondrion’s double membrane, so molecules can’t simply diffuse across and access the organelle’s insides. Mitochondria use specialized import mechanisms to take up externally made proteins. But no import mechanism exists for nucleic acids.
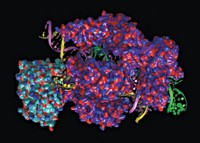
The barring of nucleic acids rules out many common gene-editing tools, such as the 2020 Nobel Prize–winning technique CRISPR, which uses a guide RNA to direct the editing machinery. Mitochondrial gene editing requires an all-protein crew.
In humans and most other animals, each mitochondrion carries 10 or so copies of circular mitochondrial DNA (mtDNA), totaling up to thousands of these genomes per cell. They can exist as a mixture of mutant copies and normal wild-type ones, a concept called heteroplasmy. Mitochondrial diseases manifest only if the fraction of mutation-bearing genomes surpasses a threshold, typically 70%. So, often the goal of mitochondrial gene editing is the reduction of the mutant mtDNA load rather than blanket correction across all genomes.
In fact, you don’t always need to edit every mutant mtDNA—or explicitly fix the faulty gene at all. There is a shortcut, stemming from the fact that mitochondria are sticklers for maintaining their genome count and can’t stand any of their circular genomes’ being broken. Any cut to one of these rings will trigger the organelle’s internal machinery to chew up the now-linear genomes and then replace them with what are usually the wild-type variants. So one promising approach to editing mtDNA takes advantage of mitochondria’s degrade-and-replace tendencies by just severing mutant genomic strands—and letting the mitochondria take care of the rest.
Cull to repair
The nuclease effect

The snip-to-supplant approach relies on old-fashioned nucleases, enzymes that cleave nucleotide chains.
Restriction endonucleases, discovered in the 1960s among bacteria, were among the earliest enzymes to be deployed for gene cloning. The same class of enzymes also became the first to find its way toward mitochondrial genetic manipulation, thanks to enzyme reengineering attempts in 2001 by Carlos T. Moraes, a geneticist at the University of Miami (Hum. Mol. Genet. 2001, DOI: 10.1093/hmg/10.26.3093).
But the application of these enzymes is quite limited. Restriction endonucleases sever DNA when they recognize certain sequences of around six base pairs. And such a short sequence has a high likelihood of appearing in the wild type too, Moraes says. “How many six-base-pairs sequences in the mitochondrial DNA do we have that’s unique?”
So far, Moraes says, only one type of mitochondrial disease is amenable to a restriction endonuclease–based therapy: neuropathy, ataxia, retinitis pigmentosa (NARP) syndrome, a neurological disorder characterized by symptoms such as muscle weakness, vision loss, and erratic sensation in the limbs. The genetic mutation behind NARP syndrome has a unique footprint that’s not present in the wild-type genome. But so far, no research group is pursuing this treatment option.
To widen the applicability of restriction endonucleases, researchers have focused on reengineering the enzymes with independent DNA-binding and DNA-cleaving components. One such restriction enzyme is FokI, whose gene recognition component can be substituted with programmable proteins such as zinc finger domains or transcription activator-like effector (TALE) motifs.
There is buzzing interest in the biotechnology industry to bring these nuclease technologies to fruition. Pretzel Therapeutics, which launched in September, is betting on zinc finger nucleases—DNA-cleaving enzymes whose gene recognition component is the zinc finger domains—to treat mitochondrial diseases. One of the company’s cofounders, University of Cambridge geneticist Michal Minczuk, has used these nucleases to correct disease-causing mitochondrial mutations in vivo (Nat. Med. 2018, DOI: 10.1038/s41591-018-0165-9). Delivered with adeno-associated viruses (AAVs), his team’s zinc finger nucleases eliminated mutant mtDNA and restored healthy heteroplasmy levels in the heart cells of live mice.
Zinc finger and TALE nucleases typically come as a dimer, or a pair. The halves need to straddle the mtDNA mutation site and then link up before they can cleave the faulty genome. Zinc finger nucleases are small enough that both monomers can fit inside a single AAV vehicle. But that’s not the case for the TALE nucleases, which require one AAV per monomer. Administering the TALE editors requires double the dose of AAVs, which may aggravate the immune system in recipients of the therapy.

Some researchers have ditched the FokI template in favor of monomer-compatible motifs, such as the algae-derived, programmable I-CreI meganuclease. The mega title may be a bit of a misnomer—the main advantage of these enzymes is that they’re small and monomeric, so each construct can be delivered with a single AAV vector. Moraes, who is working on this platform, thinks they’re also potentially more specific than zinc finger or TALE arrays.
The technology was first developed by Precision BioSciences for editing nuclear genes. A longtime Precision collaborator, Moraes is now pushing the company to adopt the technology for mitochondrial diseases and advance the editing tools into the clinic.
One downside of using genome-nicking nucleases for treating mitochondrial diseases is that for a vulnerable moment after the enzymes complete their job, the body may have little to no mtDNA left. This scenario is arguably even more dangerous than having defective mitochondrial genomes in the first place.
And whichever editor platform one chooses to wield, nucleases are helpless against homoplasmic conditions, in which all the mitochondrial genomes present contain the disease-causing mutation.
Several mitochondrial diseases, such as the blindness condition Leber hereditary optic neuropathy (LHON), are homoplasmic. In such cases, researchers need to fix the faulty genome rather than destroy it. For that, they need precision editing.
To be more precise
One balmy August day in 2018, David R. Liu, a chemist at the Broad Institute of MIT and Harvard, received an unexpected email from across the country. Joseph Mougous, a microbiologist at the University of Washington, had found a bacterium called Burkholderia cenocepacia that wreaked havoc on its victims in a curious way: it secreted a toxin that could randomly deaminate cytosine (C) nucleotides in other bacteria’s DNA, transforming them into thymines (Ts) without unraveling the double helix structure. Might Liu have an idea of what to do with a deaminase enzyme that works on double-stranded DNA?
Liu recalls thinking immediately, “Yes, in fact, I do.”
Two years earlier, his team had developed a technique for base editing the nuclear genome using a rat-sourced deaminase (Nature 2016, DOI: 10.1038/nature17946). This deaminase and subsequent iterations used CRISPR-Cas enzymes to unwind the DNA double helix before base conversion, a prerequisite for the base editors to work. The Burkholderia deaminase, known as DddA, imposed no such condition.
Liu’s phone call with Mougous led to a plan of action. In 2020, the collaborators announced the first gene correction tool that worked in mitochondria (Nature 2020, DOI: 10.1038/s41586-020-2477-4). Their editor consisted of DddA, a DNA-binding TALE group, and an enzyme that prevented the reverse reaction. To prevent indiscriminate C deamination—in Liu’s words, “tame the beast”—the researchers split the enzyme onto each of the two TALE monomers; deamination would occur only when each half landed on opposite flanks of the mutation site and reassembled into a whole.
Since the first demonstration, Liu’s group has evolved new deaminase variants that have improved mtDNA-editing efficiencies and that can convert Cs more broadly (Nat. Biotechnol. 2022, DOI: 10.1038/s41587-022-01256-8). To make the base editors more compatible with AAV delivery, the group has also replaced the TALE motifs with zinc fingers (Nat. Commun. 2022, DOI: 10.1038/s41467-022-34784-7). For now, the off-target activity is still a little too high for clinical comfort.
Other researchers also quickly figured out how to convert bases beyond Cs. Last year, researchers led by Jin-Soo Kim from the Institute for Basic Science in South Korea designed a base editor for adenine-to-guanine (A-to-G) substitution in human cell cultures (Cell 2022, DOI: 10.1016/j.cell.2022.03.039). The technology was based on a deoxyadenosine deaminase that was derived from TadA proteins in Escherichia coli bacteria.
Research is underway to cover all the bases beyond C-T and A-G switches, such as replacing C with G or A, or A with C or T. But the current C-T and A-G deaminases can already correct for 90% of clinically identified mtDNA mutations.
Liu says several companies have expressed interest in licensing the mtDNA base editor technology from Broad and the University of Washington. Discussions are underway.
One company that is already forging ahead is Primera Therapeutics, which was founded by the Mayo Clinic’s Stephen Ekker in December. Precise editing is a more logical choice than the blunt destruction wreaked by nucleases, Ekker says, because most mitochondrial gene defects are point mutations rather than wholesale deletions. Primera is banking on designer TALE deaminases to attain that precision.
Advertisement
But while base editor technology is still years away from clinical relevance, it has found a more immediate application in the laboratory: engineering animal models to carry mitochondrial mutations for preclinical testing.
Before base editing’s emergence, there were few live models with the right mitochondrial mutations. Several early tests used animals that were engineered to carry mitochondrial mutations in the nuclear genome instead. But thanks to base editing, researchers may now have an easier shot at generating more representative proxies. Ekker is leading the effort to generate more animal models, though it’s early days. “My lab has the highest density of target animal models on the planet,” he says. “We have two”—namely, two distinct genetic models in zebrafish.
But Ekker is confident that this is only the beginning. “There’s going to be a whole wave of new animal models coming out. I’m just telling you right now.”
Challenges ahead
Before mtDNA-editing therapies can make it to the clinic, they have several hurdles to clear. In fact, many of them are the same ones that plague nuclear gene editing. Ask any mitochondria researcher, and they will all home in on one answer: “There will be three key challenges,” Minczuk says. “One will be delivery, the second will be delivery, and the third will be delivery.”
Like nuclear gene editing, mtDNA manipulation raises practical concerns over how to deliver the editors to target tissues or to the entire body as needed.
Mitochondrial diseases at a glance
▸ Mitochondrion genome size: 16.6 kb; 37 genes
▸ Number of known mitochondrial diseases: >300
▸ Number of known pathogenic mitochondrial DNA mutations: 96
▸ Number of carriers of mitochondrial DNA mutations: ~1 in 200 people
▸ Mitochondrial disease prevalence: ~1 in 4,300 adults; ~1 in 6,700 children
▸ Number of children born with mitochondrial diseases each year: 1,000–4,000
Sources: Mito Foundation; Mitomap; United Mitochondrial Disease Foundation; Biochim. Biophys. Acta, Bioenerg. 2010, DOI: 10.1016/j.bbabio.2009.09.005; Ann. Neurol. 2015, DOI: 10.1002/ana.24362; Nat. Rev. Dis. Primers 2016, DOI: 10.1038/nrdp.2016.80.
Researches are also concerned about off-target activity. Editing mtDNA is a fine balance between hitting the target mitochondrial genes and avoiding the wild types and those in the nucleus. Engineering the affinity of the editors’ DNA-binding sequences is key. Experts lean toward designing iterations of recognition mechanisms that are more selective and less sticky overall.
Mitochondria are important cellular organelles, so while their associated diseases are devastating, missteps in tampering with their function can have dire consequences as well. “It’s like repairing a nuclear power plant. You need to be extremely careful,” says Vamsi Mootha, a molecular biologist at the Broad Institute and Massachusetts General Hospital. “I’m humbled by how complicated these diseases can be.”
One low-hanging fruit is the homoplasmic eye condition LHON. The mutant genes are confined to the mitochondria in the eye, simplifying the delivery problem. Moreover, the eye is immune privileged, so it can tolerate foreign substances without triggering a full-body immune cascade. But even this disorder has proved tricky to treat.
The French biotech firm GenSight Biologics has completed Phase 3 clinical trials in the US and Europe of its investigational LHON treatment. But rather than correcting the mitochondrial genome directly, GenSight’s procedure tacks the regular version of a mitochondrial NADH dehydrogenase (ND) gene to the eye’s nuclear genome. The aim is for the resulting healthy proteins to swamp the mitochondrially made mutants.
Although the clinical results were overall positive, experts doubt GenSight’s work-around. There’s a reason why the mitochondrion retained its genes for 13 proteins, including several key ND proteins, Moraes says: these hydrophobic and complex macromolecules are challenging to import and assemble in the mitochondria after they’re externally produced. “I have this skepticism because there are several layers of biology that are being challenged by this approach,” he says.
Mootha agrees. “It’s challenging to interpret their clinical results given the limited basic science studies using this technology,” he says. Last month, the European Medicines Agency gave GenSight’s investigative therapy a negative recommendation, prompting the company to withdraw it from the regulatory approval process for now.
While the world lacks an editing fix, a different approach promises to reduce the reproductive transmission of mitochondrial mutations, which are usually maternally inherited. Mitochondrial replacement therapy (MRT) does as the name suggests, replacing the majority of mitochondria in an egg cell with healthy ones by transferring over a donor cell’s cytoplasm and its contents. Children born from the procedure are often called “three-parent babies,” a term that scientists despise because mitochondrial genes have little influence on an individual’s overall genetic makeup.
Strictly speaking, MRT isn’t gene editing, but it’s regulated as if it is. The US Congress has prohibited clinical research on MRT in humans because the technique tampers with the germ line. But mitochondria scientists say that MRT shouldn’t be controversial—it’s no more gene editing than sperm donation is.
Researchers like Shoukhrat Mitalipov, an Oregon Health and Science University biologist who is a leader in developing the treatment, have no choice but to run their clinical experiments elsewhere. Mitalipov’s clinical research is taking place in Greece, with the intention of treating infertility. Clinical tests of cytoplasm replacement expressly for treating mitochondrial diseases are permitted in the UK and Australia.
Experts predict that mtDNA-editing therapies—the nucleases and base editors—will take at least a decade to get into shape, just as CRISPR needed roughly 10 years to move from concept to the clinic. Nevertheless, the rapid pace of development is thrilling because mtDNA editing is not a matter of if, but when.
“What was science fiction 3 years ago is now just hard,” Ekker says. “There’s a whole wave of new things that are going to come out in the next few years. And it’s going to scare my postdocs.”
As new tools are developed, perhaps one day it might even be possible to deliver CRISPR and its RNA component into mitochondria. “It’s a difficult [challenge], but I wouldn’t say it’s insurmountable,” Hirano of Columbia University says. “Maybe it’ll be virally mediated. Viruses get into bacteria, and we know that mitochondria evolved from bacteria.” Just as mitochondria originated from microbes, perhaps it is also from the microbial world that scientists will uncover new enzymatic possibilities.




Join the conversation
Contact the reporter
Submit a Letter to the Editor for publication
Engage with us on Twitter