Advertisement
Grab your lab coat. Let's get started
Welcome!
Welcome!
Create an account below to get 6 C&EN articles per month, receive newsletters and more - all free.
It seems this is your first time logging in online. Please enter the following information to continue.
As an ACS member you automatically get access to this site. All we need is few more details to create your reading experience.
Not you? Sign in with a different account.
Not you? Sign in with a different account.
ERROR 1
ERROR 1
ERROR 2
ERROR 2
ERROR 2
ERROR 2
ERROR 2
Password and Confirm password must match.
If you have an ACS member number, please enter it here so we can link this account to your membership. (optional)
ERROR 2
ACS values your privacy. By submitting your information, you are gaining access to C&EN and subscribing to our weekly newsletter. We use the information you provide to make your reading experience better, and we will never sell your data to third party members.
Pharmaceuticals
Viral Invasions
A small battery of drugs has been approved to treat respiratory viral infections; more are on the way
by LOUISA WRAY DALTON
May 24, 2004
| A version of this story appeared in
Volume 82, Issue 21
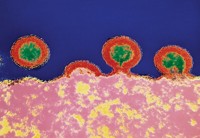
Treating a viral infection is like defending against a guerrilla strike. Viruses attack like resistance fighters. Instead of setting up camp and openly multiplying, as bacteria do, they hijack enemy cells and use the cells' own machinery to launch a new generation of resistance and new weaponry. They slip into enemy territory wearing just a simple protein capsid shell enclosing a bit of genetic instruction. They land on cells, insert the instructions, and take over.
That's why, when you go to the doctor with an itchy nose or sore throat, you hope that you are fighting a more conventional bacterial army. If so, your doctor has a whole arsenal of antibacterials to choose from.
But if your malady is viral-based--and chances are it is, because 70 to 80% of all respiratory infections are viral--more likely you will come home from the doctor empty-handed. All existing over-the-counter cough, cold, and flu medicines may help get you through the symptoms, but the virus itself is not affected by those drugs.
The AIDS epidemic and the advent of molecular biology with its tools of genetic engineering spurred much research and ushered in a burst of antivirals in the '80s and '90s. Even so, today there are only six antivirals that target respiratory viruses. The troublesome group includes influenza, parainfluenza, respiratory syncytial virus (RSV), coronaviruses (including the severe acute respiratory syndrome--SARS--coronavirus), picornaviruses (some of which cause the common cold), adenoviruses, and other still unknown respiratory-disease-causing viruses.
Treating respiratory infections presents some specific biological and economic challenges. Nevertheless, a number of strategies are in the pipeline to fight these infections. And HIV research has proven that, given the need, therapy for wily viruses can indeed be achieved.
Finding effective pharmaceutical weaponry to fend off viral attack has historically been tricky. Development of antibacterials was much more straightforward. First of all, scientists could see bacteria long before they ever saw viruses. Using his microscope, Anton van Leeuwenhoek first observed microorganisms in 1673. Most viruses are invisible under a light microscope, and it wasn't until the turn of the 20th century that viruses began to be investigated.
In addition, screening drugs against bacterial growth is relatively simple. "You just grow bacteria in some medium, throw the compound in, and then ask the question: Does it affect the growth of bacteria? You can't do that easily for viruses because viruses by themselves don't grow," says Norbert W. Bischofberger, executive vice president of R&D at Gilead Sciences. To test antiviral drugs, researchers have had to find cell cultures and animal models in which the virus replicates easily. For some viruses (such as SARS), researchers still don't have a good animal model.
Finally, "bacteria are unicellular organisms that differ from human cells very much in their makeup and in their biochemistry," Bischofberger says. Viruses perform most of their functions inside the human cell, "so it is challenging to find compounds that very specifically inhibit the virus without affecting the cell. With bacteria, that has been much easier." For example, bacteria have a cell wall made of cross-linked peptidoglycan units. Nothing of the kind exists in human cells, so drugs that inhibit bacterial cell wall synthesis in one form or another (such as penicillin and cephalosporins) are effective, safe, and broad-spectrum.

Of course, there are some targets unique to viruses. And with the advent of polymerase chain reaction and genetic engineering, those targets have become easier to find. Using just a viral genetic code, researchers can now model the structure of specific viral proteins. And using structure-based drug design, pharmaceutical makers can find a small molecule that inhibits an enzyme's activity, blocks its binding, or otherwise specifically shuts the viral enzyme down without affecting eukaryotic enzymes.
Yet each virus seems to require its own custom-designed drug. A small molecule that could inhibit all types of viruses--a pan-antiviral analogous to a broad-spectrum antibiotic--is not yet on the horizon. "I rarely use the word impossible," Bischofberger says, "but I think it's appropriate here. From what we know about viral mechanisms, I couldn't conceive of what that would look like."
The first oral antiviral was a drug for herpes, acyclovir, developed by the laboratory of Gertrude B. Elion at Burroughs-Wellcome in the 1960s. Acyclovir is a nucleoside analog that fits into the binding pocket of herpes DNA polymerase and terminates the enzyme's growing nucleic acid chain. AIDS became an issue in the 1980s, and researchers started looking for something--anything--to give dying AIDS patients. AZT, a cancer drug that became the first anti-HIV drug, was modeled after acyclovir.
Newer antiviral drugs, primarily anti-HIV agents, target other steps in the viral life cycle. Some attempt to block the initial binding of virus to receptors on the cell surface, and some block the fusion of viral envelope with the cell membrane. A number of drugs target the proteins encoded by the viral genetic material that are made once the virus has started directing cellular activity. For example, viral polymerases create viral nucleic acids, and viral proteases cut apart the newly created polypeptides.
Respiratory viral targets aren't yet as well known as HIV targets, although diseases caused by influenza virus and RSV cause significant death and disease. "If you look at commercial interest," Bischofberger says, "there are first the herpes viruses, and that was addressed by acyclovir, at least partly. And then there were the retroviruses, including HIV. And the last holdout is the respiratory viruses." There are reasons for that situation.
Biologically, respiratory viruses are challenging to treat. First, the treatment window is narrow. After initial infection, respiratory viruses replicate rapidly. Quickly, "the density of virus in the nasal cavity grows exponentially, on the order of 12 to 24 hours," says Siegfried Reich, head of viral and ophthalmic diseases at Pfizer, La Jolla, Calif. And the body responds with a strong immune defense. "It's almost like an overreaction," Reich says. Most of what we identify with a respiratory infection--the sneezing, the congestion, the runny nose--is "really an extreme immune response to an invader." The viral load often decreases after a few days, while a cascade of trailing sniffles and leftover cough may last for weeks. Therefore, a treatment, to be effective, must get at the virus early--within 24 to 48 hours of onset of symptoms.
Second, respiratory viruses can be vastly different from each other, yet the symptoms that they cause are almost indistinguishable. "Take, for instance, the commonly known influenza, parainfluenza, respiratory syncytial virus, and coronavirus," Bischofberger says. "The disease symptoms are the same: cough, fever, muscle ache. You know how you feel when you have the flu. It's just called the flu." Yet in fact, it could have been caused by any number of viruses. The only thing, really, that keeps respiratory viruses in the same category is this similar clinical manifestation. Respiratory viruses, according to Reich, just "happen to replicate very nicely" in the respiratory tract (the lungs, epithelial tissue, and nasal cavity).
The trouble is that a drug designed to inhibit the parainfluenza polymerase probably would do nothing against a coronavirus polymerase and vice versa. Without knowing which virus is the troublemaker, treatment is hit-or-miss.
INFLUENZA. Influenza tends to be easier to pick out of the crowd than the others. "You can tell when the flu epidemic is on the march," says Greg Tannock, professor of virology at RMIT University in Melbourne, Australia. It is a seasonal disease. During flu season and in a community experiencing an outbreak, the percentage of respiratory illnesses attributable to influenza is well over 50%.
That pattern certainly makes it easier to perform a clinical trial, and perhaps that is why influenza now has the best antiviral arsenal of all the respiratory diseases. Four drugs are available that specifically target influenza.
Two older drugs, amantadine (Symmetrel) and its derivative rimantadine (Flumadine), fight just the influenza A virus. (Influenza comes in many subtypes, but A and B are the primary categories that cause human disease.) These symmetric tricyclic amine compounds interfere with proton transport of the viral transmembrane protein called M2.
Two newer and broader drugs are also available: the neuraminidase inhibitors, oseltamivir (Tamiflu) and zanamivir (Relenza).
"Flu is an enormous problem," says Gilead's Bischofberger, who helped develop Tamiflu. According to the Centers for Disease Control & Prevention, 10 to 20% of the population is infected every year. And then a pandemic rolls around about every 25 years, Bischofberger says. Gilead scientists knew they wanted to develop an influenza drug that would be effective against as many strains of influenza as possible because the virus mutates yearly. "Influenza replicates in three main species: pigs, birds, and humans. And viruses from the three species can rearrange," Bischofberger says. In addition, the scientists knew they needed to target a portion of the virus that was essential to its function. Otherwise, a resistant version could easily arise.
The scientists chose the neuraminidase enzyme. When influenza viruses land on human cells, one of the outer viral glycoproteins, hemagglutinin, binds to the sialic acids found on the outside of all human cells. This works well the first go-round, but when new viruses bud off the human cell, they're enclosed in human membrane, and sialic acid is now part of their own coat as well. Newly formed viruses would clump together if it weren't for a second viral membrane glycoprotein, the neuraminidase enzyme. This enzyme clips off sialic acid from newly formed viral particles, freeing them from clumping and allowing them to bind to new human cells.

The Gilead team used structure-based drug design to develop oseltamivir, which blocks the active site of neuraminidase.
Successful neuraminidase inhibitors have inspired the development of new ones, and a number of companies have candidates in the pipeline, Tannock says.
Because the effectiveness of oseltamivir depends on receiving the drug as soon as possible after infection, Gilead has explored the administration of the drug even before infection, as a preventive agent, and oseltamivir is approved for prophylactic use. "I think the most likely use would be what we call 'post-exposure prophylaxis,' " Bischofberger says. When one member of the household gets sick, all others start taking Tamiflu. "In my mind, that would be the best use of our drug."
The ultimate in preventive therapy against viruses is, of course, vaccination. One or two shots before initial exposure can protect an individual for years or even for life because the immune system builds up antibodies against the weakened or dead virus in the vaccine. But some respiratory viruses, including influenza and rhinoviruses, mutate so rapidly that a vaccine's effectiveness expires quickly. Because influenza is such a threat, a new influenza vaccine is re-created every year, and that vaccine is a strong protection for the old, the young, and the immunocompromised. Unfortunately, sometimes, like this year, the vaccine makers incorrectly predict which strain will dominate. In addition, Tannock says, "it's hard to develop an effective immune response in the respiratory tract." The immunity often doesn't last long.
RSV. Physicians would love to have a vaccine for the infection that is the major cause of lower respiratory tract disease in infants and children: respiratory syncytial virus. RSV is the number-one reason why babies under one year old are hospitalized in the U.S., according to Alan Cohen, a pediatrician and senior director of medical affairs at MedImmune. A formalin-killed vaccine was actually created in the 1960s against RSV. But when tested, it backfired. Children who received the vaccine, when subsequently exposed to live virus, developed even more severe symptoms than children who received no vaccine.
Researchers now think that the vaccine actually helped prime the part of the host immune response that contributes to an RSV infection (the Th2 subclass of helper T cells). "It basically revved up the immune response so that when children were exposed to the real virus, it unleashed a more dangerous response," Cohen says. Creating a vaccine that avoids priming this part of the immune response while supporting the immunity-building response has been tricky. The National Institutes of Health "has been working on a program for about 30 years," Tannock says. "I think a drug is the only answer for RSV."
Advertisement
Two antivirals are approved by the Food & Drug Administration for use against RSV: ribavirin and palivizumab.
Ribavirin is a purine nucleoside analog that was first synthesized in 1970 and was shown to have some general antiviral effects in 1972. It is effective in combination therapy against the hepatitis C virus and was actually one of the first drugs tried when SARS began to emerge, although it was quickly found to be ineffective against SARS.
Ribavirin's mechanism of action is not well understood. In vitro, it does not act as a direct antiviral. Some suspect that it boosts the human immune response or encourages a mutating virus to mutate too much. The treatment is cumbersome and expensive, according to Janet England, associate professor of pediatric infectious disease at the University of Washington Children's Hospital and Regional Medical Center in Seattle, Washington. "Ribavirin is available, and it is used, but not very much," she says.
One other preventive treatment option currently exists for RSV: MedImmune makes a human monoclonal antibody: palivizumab (or Synagis). Approved by FDA in 1998, Synagis is a genetically engineered antibody specific to a highly conserved glycoprotein on the surface of the respiratory syncytial virus: the F protein (F because it helps with fusion). "It was the first monoclonal antibody approved for use in humans to protect against any kind of infection," Cohen says.
Antibody therapy is somewhere in between a vaccine and a drug. Instead of priming the immune system to create its own antibodies against a certain disease, antibody therapy provides prefabricated antibodies. Babies receive the same kind of short-term immune help from a mother's antibodies in breast milk.
Synagis must be taken before exposure, so it is injected into muscle on a monthly basis during the RSV season, and it is primarily prescribed for premature infants and other high-risk babies. Expensive monthly shots aren't for every child, but because it is taken beforehand, antibody therapy does bypass the problem of getting the drug in the first 48 hours of symptom onset, Cohen notes.
On the research front, a few anti-RSV compounds have shown some activity both in vitro and in cotton rats.
Parainfluenza virus is also of particular concern for children, and a newly discovered virus, the metapneumovirus, which was first described in humans in 2001, may be another agent to which children are especially susceptible. Neither virus has any approved antiviral. Metapneumovirus has actually been around a long time. But because many low-lying respiratory viruses go undiagnosed, it was not recognized until recently.
SARS. Unlike metapneumovirus, other viruses are enough of a problem from their first appearance in humans that they demand research attention. The SARS viral genome, for example, was entirely sequenced within three or four months of the SARS outbreak in China last year.
Many academic laboratories and some companies are now working on leads for an anti-SARS drug. To be truthful, an antiviral for SARS will likely not be a big moneymaker, Pfizer's Reich says. SARS may, however, become a significant public health concern, and Pfizer is one of the main pursuers of a SARS antiviral.
Pfizer got somewhat of a jump-start when Rolf Hilgenfeld, director of the Institute of Biochemistry at the University of Lübeck, in Germany, described the first crystal structure of a coronavirus protein: the main protease, also called the 3C-like protease. Pfizer had been actively working to develop an inhibitor for picornaviruses (a possible treatment for the common cold), and one of their molecules looked like it might fit very nicely inside the active site of the SARS protease.
It turns out that this molecule, ruprintrivir (C&EN, May 19, 2003, page 13), is not an effective drug against either picornaviruses or SARS coronavirus. However, Pfizer was able to leverage a great deal of its work on picornaviral infections toward creating a new SARS program. At the moment, they are pursuing drug candidates that inhibit the SARS protease.
Hilgenfeld and collaborators in Beijing and Shanghai continue to characterize more SARS proteins that may be good targets for antiviral therapy--for example, the RNA-dependent RNA polymerase and SARS helicase (which helps unwind the viral genetic material). They are also elucidating the structure of proteins whose function is still unclear.
"The approach that we follow is really a structural genomics approach," Hilgenfeld says. "The problem is, this virus has a very big genome for an RNA virus: 30,000 bases. It is the largest RNA genome known. It is quite dynamic. During evolution, these coronaviruses sometimes lose genes and proteins or then they make new ones, and no one knows what they are good for." SARS makes between 22 and 28 proteins, Hilgenfeld says, "but we only know the function of a handful of them."
Other laboratories are exploring different anti-SARS coronavirus strategies. One strategy is to use heptad repeats as fusion inhibitors, mimicking one of the most recent tacks in anti-HIV therapy. The protein that gives coronaviruses their name is called the spike protein. It sticks out from the surface like a halo--or a corona during a total eclipse of the sun. This protein is responsible for binding and fusing with human cells, and it has a recurring seven-repeat sequence in a triple-helix coil. "The idea is to synthesize peptides which correspond to these heptad repeats," Hilgenfeld says. "It has been shown, at least for HIV--and I am convinced it will work for SARS--that these heptad-repeat-derived peptides compete with the virus for binding to the receptor."
Interferons also are candidates for an anti-SARS drug. These glycoproteins, produced naturally by the human body, are not directly antiviral. Yet a shot of recombinant human interferon does help the immune system fight a number of maladies, including viral infection. All three types-- ,β , and
,β , and  --are already FDA approved to fight other illnesses, including hepatitis C, cancer, and multiple sclerosis.
--are already FDA approved to fight other illnesses, including hepatitis C, cancer, and multiple sclerosis.
Interferons "are like the Paul Revere of the cell," says Dale Barnard, a professor of microbiology at Utah State University. Once a virus has taken over a cell and starts to make double-stranded RNA or a DNA/RNA hybrid, the defeated human cell begins to make interferons. Interferons then leave the cell and bind to neighboring uninfected cells, triggering the production of antiviral proteins. "Interferon is the warning messenger," Barnard says.
Barnard is affiliated with Utah State's Institute for Antiviral Research, which is led by Robert W. Sidwell. The institute is one of two facilities in the U.S. that has funding from the National Institute of Allergy & Infectious Diseases to screen anti-SARS compounds in cell culture. Utah and the Southern Research Institute (SRI) in Birmingham, Ala., receive compounds from across the U.S. for initial screening in African green monkey kidney cells.
"As far as what we have been sent," Barnard says, "the interferons have been the most potent and the most reliable. Plus, many are already FDA approved" and could be quickly put to use in SARS patients. Barnard qualifies, however, that none of them has been tested in animal models. In fact, a good animal model for SARS that reflects how the virus causes disease in humans does not yet exist, although SRI and others are actively working to create one.
COMMON COLD. The common cold, caused by a number of strains of picornaviruses (rhino- and enteroviruses) has, so far, eluded the reach of any antiviral drug, in part because any drug that FDA approves for a non-life-threatening disease must be "very, very safe," says Jack Secrist, vice president for drug discovery at SRI.
Pleconaril, a drug candidate made by ViroPharma, is one compound that recently made it to Phase III clinical trials for treatment of the common cold. This molecule fits into a hydrophobic pocket on the capsid of rhinoviruses and enteroviruses and blocks attachment and uncoating of the virus.
In 2002, the FDA advisory committee for antiviral drugs reviewed a tablet version of pleconaril. "It did appear that it had some efficacy--about a half a day or a day's reduction in cold symptoms, but as it turned out, it had a pretty pronounced drug interaction with birth control pills, making the birth control perhaps ineffective," says Jeff Murray, deputy director of the division of antiviral drug products at FDA's Center for Drug Evaluation & Research. "And for a self-limiting illness like a cold, the drugs need to be squeaky clean. For a drug that would perhaps result in unwanted pregnancies, the risk/benefit was considered not to be favorable." ViroPharma has reformulated pleconaril and entered into an agreement with Schering-Plough to market an intranasal version of the drug, which would limit its interaction with other drugs.

ECONOMIC CONSIDERATIONS. The challenges of developing drugs for respiratory illnesses are not only scientific but also economic and political. "I think antiviral drugs have a role," Tannock says. "But they won't be cheap." Developing an antiviral drug that specifically inhibits one protein in one type of virus and performing clinical trials on that drug are expensive. Treatment with Tamiflu costs $50 for a child and $75 for an adult.
Advertisement
In Europe and other places with socialized health care, the prospects for antiviral drugs are particularly dim, Tannock says. Governments do not have a lot of money for antivirals--especially for respiratory infections, which are hard to distinguish from each other and tend to be self-limiting illnesses.
When Gilead approached some European governments about offering Tamiflu in their countries, the idea wasn't so warmly welcomed. "This was never explicitly said," Bischofberger says, "but we were met a little bit with the sentiment, 'Oh this is just going to cost us a lot of money. We'll just deal with it with chicken soup--it's cheaper than having a prescription medication used broadly for the whole population.' That's not an issue in the U.S. It's all a market economy. But in Europe, some governments were not jumping up and down. They thought it would cost them a lot of additional money. If [the drug] is broadly used in a flu season for prophylaxis, [the cost] adds up. And it is money that these health care systems don't have."
Bischofberger adds that the needs of public health sometimes don't mesh with the commercial realities of pharmaceutical companies. "If you look at public health, it would probably be worthwhile to have a coronavirus agent," he says. But because coronaviruses cause only a minority of all respiratory infections, you would probably need a diagnostic test to distinguish coronavirus from all other respiratory viruses. "And if you need a diagnostic, you have to think about the costs and the administration," he continues. The test "should be quick. It should be at the doctor's office. It really complicates things. A pharmaceutical company developing a coronavirus agent may not be able to recoup the costs associated with bringing a drug to the market."
Antiviral drug development is costly and takes a lot of perseverance, agrees Pfizer's Reich, but for a chemist, this combination presents an exciting opportunity. "There aren't a whole slew of viral targets out there. And then when you get to doing structure-based design on them, they can be quite challenging." The HIV protease inhibitors, for example, have multiple asymmetric centers, and lots of effort went into conquering those viral targets.
"In the early days," Reich says, "viruses seemed horrendous. They mutate. In the case of the respiratory viruses, they have this immune response. But major milestones have been reached in getting antiviral compounds to the marketplace in spite of all the challenges. Antiviral drug research is a great testing ground for chemists--if you're up for it."








Join the conversation
Contact the reporter
Submit a Letter to the Editor for publication
Engage with us on Twitter