Advertisement
Grab your lab coat. Let's get started
Welcome!
Welcome!
Create an account below to get 6 C&EN articles per month, receive newsletters and more - all free.
It seems this is your first time logging in online. Please enter the following information to continue.
As an ACS member you automatically get access to this site. All we need is few more details to create your reading experience.
Not you? Sign in with a different account.
Not you? Sign in with a different account.
ERROR 1
ERROR 1
ERROR 2
ERROR 2
ERROR 2
ERROR 2
ERROR 2
Password and Confirm password must match.
If you have an ACS member number, please enter it here so we can link this account to your membership. (optional)
ERROR 2
ACS values your privacy. By submitting your information, you are gaining access to C&EN and subscribing to our weekly newsletter. We use the information you provide to make your reading experience better, and we will never sell your data to third party members.
Environment
Polymers Exploited for Drug Delivery
ACS MEETING NEWS: Biocompatibility and biodegradability are key elements in design of polymers for therapeutics
by MICHAEL FREEMANTLE, C&EN LONDON
April 18, 2005
| A version of this story appeared in
Volume 83, Issue 16

Polymeric materials are playing increasingly important roles in the development of novel medical devices and drug delivery systems.
"Polymer science and engineering have enabled the explosive growth in the medical device industry, particularly in therapeutic-device combination products," noted Shrirang V. Ranade, a senior research scientist at the medical device company Boston Scientific, in Natick, Mass. Ranade co-organized a symposium on the topic sponsored by the Division of Polymeric Materials: Science & Engineering at last month's national meeting of the American Chemical Society in San Diego. The other co-organizer was Signe E. Varner, director of ocular drug delivery for Doheny Retina Institute and Keck School of Medicine at the University of Southern California, Los Angeles.
Biocompatibility is a key functional requirement of the next generation of medical devices and drug delivery systems, according to Michael N. Helmus, vice president for advanced biomaterials at Boston Scientific. "Biocompatibility of biomaterials has traditionally been viewed as a requirement that must be met in order to market a safe medical device or delivery system," he remarked. "With the emergence of complex combination products, a paradigm shift is occurring that now requires biocompatibility to be designed into the device."
Helmus explained that the view that biocompatible materials should "do no harm"--that is, they should be, for example, nontoxic, nonantigenic, and nonmutagenic--is changing to the view that such materials should "do good" by encouraging positive healing responses.
One of the main areas of interest at the symposium was the development and improvement of biocompatible delivery systems using existing polymeric materials and the development of new polymers with specific or improved properties for therapeutic delivery.
Ranade, for example, presented a paper on the controlled delivery of paclitaxel (Taxol) from cardiac stent coatings made of newly modified versions of styrene-isobutylene block copolymers. Cardiac stents--wire mesh tubes placed in arteries to hold them open--are susceptible to restenosis, a process in which vascular smooth-muscle cells migrate to cover the devices. In many cases, layers of tissue build up around the stent, resulting in the narrowing of arteries and occlusion of blood flow. Paclitaxel, an antiproliferative drug most widely used for treating ovarian and other types of cancer, prevents restenosis. It inhibits cell division and migration by binding to and stabilizing hollow protein subunits of the cells known as microtubules.
THE NEW COPOLYMERS described by Ranade are hydroxylated and acetylated derivatives of poly(styrene-b-isobutylene-b-styrene) (SIBS). Joseph P. Kennedy, distinguished professor of polymer science and chemistry at the University of Akron, in Ohio, first reported the synthesis of SIBS in 1986. The material is a soft thermoplastic elastomer that consists of polyisobutylene blocks flanked by "hard" blocks of polystyrene that have a glass transition temperature much higher than room temperature. The two components separate as microphases in the material. The way they separate--as spherical, lamellar, or cylindrical structures, for example--and the mechanical properties of SIBS depend on the relative weight percentage of polyisobutylene and polystyrene in the material.
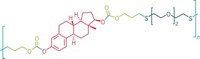
The triblock polymer is used in a commercial paclitaxel-eluting SIBS stent device developed by Boston Scientific. The device was approved for human use in the European Union in January 2003. The stent consists of stainless steel with a SIBS drug delivery coating that administers the paclitaxel. Last year, Ranade, Helmus, and coworkers showed that the drug exists as discrete particles embedded in the polymer matrix (J. Biomed. Mater. Res. 2004, 71A, 625).
Helmus remarked that Boston Scientific's drug-eluting stent is an example of a device that applies the concept of enhanced biocompatibility. The stent provides the mechanical function of the original design and also has a pharmacological agent in its coating that inhibits restenosis.
Ranade observed that SIBS has excellent biostability and mechanical properties that derive from its phase-separated block copolymer morphology. The release of paclitaxel from SIBS can be modulated either by adjusting the drug-loading ratio or by modifying the triblock morphology using a polymer blending approach, he explained.
IN COLLABORATION with chemistry professor Rudolf P. Faust at the University of Massachusetts, Lowell, Ranade and coworkers are continuing to develop new polyisobutylene-based drug delivery matrices by changing the chemical character of the hard blocks. "These new polymers can provide a wide variety of paclitaxel release profiles," Ranade said.
At the San Diego meeting, Ranade presented preliminary results on the release of paclitaxel using poly(hydroxystyrene-b-isobutylene-b-hydroxystyrene) and its acetylated derivative. "The hydroxystyrene and acetoxystyrene triblock copolymers have appropriate mechanical properties for use as drug delivery coatings for coronary stent applications," Ranade noted. In both cases, he added, the release of paclitaxel is significantly faster than from the SIBS block copolymer, which indicates that the polarity of the derivatives increases drug/polymer miscibility and therefore enhances the release of paclitaxel from the polymers.
Historically, there has been intense interest in the use of biodegradable polyesters such as poly(lactic acid)s (PLAs), poly(glycolic acid)s (PGAs), and their copolymers, poly(lactic-co-glycolic acid)s (PLGAs), as carriers for drug delivery. They degrade by hydrolysis, releasing drugs that have been mixed into them. The polymers themselves provide no inherent therapeutic benefit but are biocompatible in the "do no harm" sense to the extent that their degradation products, lactic acid and glycolic acid, are removed from the body. The acidic breakdown products, however, can cause local inflammation if the polymers are used for site-specific drug delivery applications such as cardiac stents. In addition, when the polymers degrade, they can break up into fragments or particulates in a process known as bulk erosion. This process results in an erratic release of the drugs within the body.
At the ACS meeting, Huashi (Ted) Zhang, director of polymer development at MediVas, San Diego, described a novel family of bioabsorbable polymer coatings that overcome these limitations. "We have developed novel amino acid-based poly(ester amide) copolymers [PEAs] as coating materials for drug-eluting stent applications," Zhang explained. "PEAs are prepared under mild solution polymerization conditions, are devoid of toxic catalysts, and have reproducible molecular weights. They exhibit excellent blood and tissue compatibility, as demonstrated in vitro in cell culture and in vivo in preclinical porcine model studies and a human safety trial. Their high elasticity and good film-forming properties make PEAs excellent coating materials for drug-eluting stents."
The PEAs developed by MediVas contain the amino acids L-lysine and L-leucine and have a proteinlike composition with carbonyl ester and amide linkages.
PEAs are fully biodegradable and do not induce an inflammatory or immune response when processed by cells, MediVas Chief Scientific Officer Bill Turnell told C&EN. "They do not degrade by hydrolytic bulk erosion like PLAs, PGAs, and PLGAs, but by enzymatic surface erosion," he said. "Enzymes produced by the body's clearance cells recognize specific amino acids in the polymers. The resulting erosion process facilitates steady and controlled release of drugs or biologics."
The polymers can also be programmed for different drug delivery applications. Desired physical properties of the materials are obtained by selecting different components that make up the polymer backbone. The materials can also be combined with drugs in different ways. Mechanical mixing of a drug and a PEA results in a matrix material that allows the release of the drug to be controlled by diffusion. Alternatively, drugs can be conjugated to the polymers by covalent attachment and released by polymer biodegradation once they reach their targets.
"Our in-house matrixing and conjugation chemistries allow us to deliver drugs and biologics from a device or from a particle with the specific sustained-release profile required for that particular application," explained Sonya Summerour Clemmons, director of business development at MediVas.
One of the company's polymers, she pointed out, has been licensed by both Boston Scientific and the cardiovascular medical device company Guidant for their next generation of drug-eluting stent delivery devices. In another MediVas program, PEAs are currently being used in two animal trials for the sustained delivery of small-molecule drugs to the back of the eye. MediVas' polymers can also be used to produce PEA nano- and microparticles for tissue-targeted drug delivery and for the delivery of biologics such as antisense molecules--single- or double-stranded RNA or DNA--into cells without the use of viral or other vectors or adjuvants.
"Multiple constructs of the same polymer class have been used to deliver therapeutics ranging from highly hydrophobic small molecules such as the sirolimus family of drugs to highly hydrophilic compounds such as proteins and protein fragments," Clemmons added. "We have, for example, an immunology program geared toward producing therapeutic peptide vaccines. Our polymers have the ability to be engulfed and digested by antigen-presenting cells. By attaching disease-specific antigens to the polymer, it is possible to induce strong immune responses against diseases such as AIDS and various types of cancer."
AT RUTGERS University, Piscataway, associate professor of chemistry Kathryn E. Uhrich and coworkers have developed a polymerization technology that enables a drug to be its own biodegradable delivery vehicle. These "self-delivering drugs" are transported more efficiently and at higher concentrations than conventional polymer carriers and can be delivered to specific sites in the body, according to Uhrich. The drugs are based on a family of poly(anhydride esters) that degrade into therapeutically active molecules.
"Poly(anhydride esters) are biocompatible polymers," Uhrich explained. "They are essentially polymeric prodrugs. They degrade hydrolytically into nonsteroidal anti-inflammatory drugs (NSAIDs) such as salicylic acid, just as aspirin (acetylsalicylic acid) hydrolyzes into salicylic acid upon ingestion. The function of the polymers is twofold: They serve as a temporary barrier between tissues, and the degradation products of the polymers locally influence the inflammatory process."
One such polymeric prodrug, dubbed PolyAspirin, is based on carboxyphenoxydecanoate. The drug hydrolyzes most rapidly in a basic environment to form salicyclic acid and sebacic acid [HO2C(CH2)8CO2H], which is excreted. Unlike aspirin, which can damage stomach lining and cause bleeding and stomach ulcers following prolonged use, PolyAspirin passes through the stomach's acidic environment to the patient's lower intestine, where the environment is more basic. The polymeric nature of the drug also allows it to be formed into fibers by extrusion, microspheres by emulsion-precipitation methods, and films by solvent casting. Such processes enable drugs to be produced that can be used for localized drug delivery--for example, on cardiac stents.
The synthesis and degradation characteristics of PolyAspirin were first described several years ago by Uhrich and graduate student Laura Erdmann (Biomaterials 2000, 21, 1941). They prepared the polymers by melt condensation polymerization of benzyl salicylate and sebacoyl chloride [ClCO(CH2)8COCl].
The properties of poly(anhydride esters) also facilitate a two-pronged approach to drug delivery. For example, antibiotics such as tetracycline can be physically admixed with the polymers for the delivery of two drugs. The tetracycline is released by erosion of the polymer's surface; the salicylic acid, by hydrolysis of the polymer backbone.
"We are building upon our progress by developing new therapeutic NSAID-based polymers (PolyNSAIDs) that can address periodontal indications, deep bone infections, restenosis, inflammatory bowel disease, and other related inflammatory diseases," Uhrich said. "We are currently evaluating the ability of these polymers to simultaneously reduce inflammation, control pain, and eliminate bacteria."
IN RECENT WORK using animal models, Uhrich; Robert D. Harten, assistant professor of orthopedics at New Jersey Medical School, Newark; and their coworkers evaluated the effect of PolyAspirin formulations on healing bone defects (J. Biomed. Mater. Res. 2005, 72A, 354). The results indicate that salicylic acid-releasing poly(anhydride ester) microspheres can locally inhibit both bone loss and bone formation in vivo. "Clearly, however, additional work is needed to evaluate longer term effects and the tissue response to varied 'doses' for treating bone injuries," the authors noted. "Regardless, these data suggest that this biodegradable polymer may be clinically useful where bone formation is not desirable and for limiting regions of local bone lysis."
In another paper, the Rutgers team describes the synthesis and cytotoxicity of a series of seven new poly(anhydride esters) based on salicylate derivatives, including halogenated salicylates, aminosalicylates, salicylsalicylic acid, and thiolsalicylic acid (Biomacromolecules 2005, 6, 359). "We conclude that the NSAIDs could all be made into polymers and that the polymers are both biodegradable and biocompatible," Uhrich told C&EN.
In 2000, Uhrich cofounded the New Jersey-based start-up company Polymerix to commercialize the PolymerDrug technology developed at Rutgers. In 2003, Polymerix entered into a partnership with Boston Scientific for several medical device applications.
Advertisement
Polymerix's PolyAspirin is currently in preclinical development following successful porcine model studies and is scheduled to enter clinical trials later this year. Polymerix is also developing PolyNSAID microspheres to treat arthritis, postoperative pain, and sports injuries.








Join the conversation
Contact the reporter
Submit a Letter to the Editor for publication
Engage with us on Twitter