Advertisement
Grab your lab coat. Let's get started
Welcome!
Welcome!
Create an account below to get 6 C&EN articles per month, receive newsletters and more - all free.
It seems this is your first time logging in online. Please enter the following information to continue.
As an ACS member you automatically get access to this site. All we need is few more details to create your reading experience.
Not you? Sign in with a different account.
Not you? Sign in with a different account.
ERROR 1
ERROR 1
ERROR 2
ERROR 2
ERROR 2
ERROR 2
ERROR 2
Password and Confirm password must match.
If you have an ACS member number, please enter it here so we can link this account to your membership. (optional)
ERROR 2
ACS values your privacy. By submitting your information, you are gaining access to C&EN and subscribing to our weekly newsletter. We use the information you provide to make your reading experience better, and we will never sell your data to third party members.
Biological Chemistry
Pain Relief From Snail Spit
Scientists engineer an orally active conotoxin
by Bethany Halford
July 26, 2010
| A version of this story appeared in
Volume 88, Issue 30

Sea snails are not known for their speed. So to snare a meal of agile fish, marine cone snails have evolved an arsenal of chemical weapons. The mollusks use a deadly dose of conotoxins—peptide toxins that disrupt myriad biological functions—that they inject into passing prey with hypodermic-needle-like teeth that shoot from their mouths like harpoons.
Within the conotoxin brew are several peptides that relieve tough-to-treat neuropathic pain just as well as morphine does but without its addictive properties. Although scientists have tried to turn such compounds into pain relievers, they’ve been hamstrung with problems administering such drugs. The pain reliever Prialt, for example, is a synthetic version of ω-conotoxin MVIIA, but it must be injected directly into the spinal cord with a surgically implanted pump.
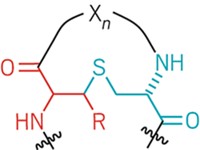
Now, scientists in Australia have managed to engineer a conotoxin that can be taken orally. Researchers led by David J. Craik of the Institute for Molecular Bioscience at the University of Queensland discovered that by linking the N-terminus of α-conotoxin Vc1.1—a compound derived from Conus victoriae—to its C-terminus, they could make the 16-residue peptide orally active (Angew. Chem. Int. Ed., DOI: 10.1002/anie.201000620).
In the cyclized peptide, which is known as α-conotoxin cVc1.1, the protein’s head and tail are tethered by a string of six amino acids—two alanines flanked on each side by two glycines. Craik says he chose the linker because it was inexpensive, wouldn’t add any functionality to the molecule, and would be easy to characterize with nuclear magnetic resonance. In tests with rats, the cyclized peptide proved to be as potent a painkiller as gabapentin, the most popular drug for neuropathic pain, even though the conotoxin-based peptide was administered at a dose that is less than 1% of the dose typically given for gabapentin.
“For years people have been saying that peptides make fantastic drug leads because they’re very potent,” Craik explains. “The problem is that they’re generally regarded as poor drugs because they’re not stable and they’re not orally available, so the pharmaceutical industry has kind of shied away from peptides in the past.”
There are, in fact, very few peptide drugs that can be taken orally. The immunosuppressant cyclosporine, a cyclic peptide made of 11 amino acids, is one example, but it’s relatively small compared with most potential protein therapeutics.
Craik’s group has shown that cyclizing larger peptides can make them orally available. “All you need is for the ends to be roughly close to one another,” he says. His team’s analysis of the protein database shows that up to 25% of all proteins have their ends within 10 Å of one another—a distance that could easily be spanned with linkers of six to 10 amino acids.

Tying the ends of a protein together makes the molecule resistant to exopeptidase enzymes that chomp away at peptide termini. But Craik says the cyclization also enhances hydrogen bonding across the entire molecule, making it resistant to the endopeptidases that attack a protein’s interior amino acids. He says it’s sort of like a zipper: “A zipper can be regarded as a series of hydrogen bonds all interlocking together, and when you zip it all up, you’ve got a beautiful set of coordinated hydrogen bonds. But you’ve still got two ends, and when you pull apart those two ends of the zipper, then the first hydrogen bond goes, then the next, and then the next.”
So if you could padlock the ends, you’d stop the protein’s ability to unzip. “It’s a crude analogy but I think it does apply to proteins,” Craik continues. “If you can work out where the weak point is, and lock it somehow so that it can’t unravel, then it synergistically helps the rest of the molecule to be more stable. And that, in turn, increases hydrogen-bonding strength and makes the molecule less susceptible to proteolysis.” Disulfide bonds within the peptide also provide stabilization.
Cyclization isn’t the only way to lock down a peptide and enhance its stability. Some chemists have also used chemical braces to link amino acid side chains together (C&EN, June 2, 2008, page 18), and others have used salt bridges between ionic residues or coordination to metal ions. Cyclization, however, is conceptually and synthetically much simpler—just lash the head to the tail.
“Nature discovered this concept of cyclization long before we did,” Craik points out. One example, the cyclic peptide kalata B1, was discovered in the 1970s by Lorents Gran, a Norwegian doctor who was working in the Congo region of Africa. Gran noticed that the local women drank a certain tea when they were about to give birth and this seemed to shorten their time in labor. He identified the protein from the native plant used to make the tea that was responsible for the uterotonic effects.
Kalata B1’s structure, however, remained a mystery until the 1990s, when Craik became aware of Gran’s work. “I thought, well, if this peptide can be boiled and then orally ingested and still have uterotonic effects, it must have an interesting structure,” he recalls. “Most peptides would break down when you boil them and certainly wouldn’t be orally available.” He found that the 29-amino-acid peptide possessed a head-to-tail cyclic backbone with a knotted arrangement of disulfide bonds.
Since then, Craik has discovered several other examples of cyclic peptides, which he calls cyclotides (C&EN, April 19, 2004, page 40). He’s hoping to use their structural features to guide the engineering of other peptides, as he did with α-conotoxin cVc1.1.
Craik’s cyclized conotoxin “is a prime example of how peptide bioengineering can enhance bioavailability,” comments Jon-Paul Bingham, a professor of molecular biosciences and bioengineering at the University of Hawaii, Manoa, noting that an orally active drug with the painkilling power of Prialt “would absolutely revolutionize how we manage chronic and terminal pain.”
At the moment, Craik is trying to raise funds so enough preliminary experiments can be done to file an Investigational New Drug Application. “The most challenging aspect has been just raising the money to get it commercialized,” he says. “Pharmaceutical companies are always a little nervous about peptides. We need more success stories so that they’ll see peptides not only as fantastic leads but also as potential drugs.”




Join the conversation
Contact the reporter
Submit a Letter to the Editor for publication
Engage with us on Twitter