Advertisement
Grab your lab coat. Let's get started
Welcome!
Welcome!
Create an account below to get 6 C&EN articles per month, receive newsletters and more - all free.
It seems this is your first time logging in online. Please enter the following information to continue.
As an ACS member you automatically get access to this site. All we need is few more details to create your reading experience.
Not you? Sign in with a different account.
Not you? Sign in with a different account.
ERROR 1
ERROR 1
ERROR 2
ERROR 2
ERROR 2
ERROR 2
ERROR 2
Password and Confirm password must match.
If you have an ACS member number, please enter it here so we can link this account to your membership. (optional)
ERROR 2
ACS values your privacy. By submitting your information, you are gaining access to C&EN and subscribing to our weekly newsletter. We use the information you provide to make your reading experience better, and we will never sell your data to third party members.
Materials
Graphene Oxide Balm Treats Skin Tumors
Cancer Therapy: A biopolymer helps graphene oxide penetrate skin and accumulate inside tumors, where laser light can heat up the material to kill cancer cells
by Prachi Patel
January 16, 2014

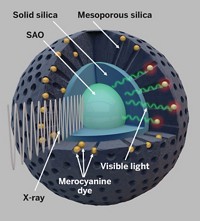
By harnessing a common biological polymer found in skin and skin care products, researchers have delivered possibly therapeutic nanoparticles of graphene oxide through the skin and into melanoma tumors in mice(ACS Nano 2014, DOI: 10.1021/nn405383a). Irradiating the tumors with near-infrared light causes the particles to generate heat that destroys the surrounding cancer cells. As a potential skin cancer therapy, delivering graphene oxide locally, as opposed to intravenously, would cause fewer side effects, the researchers say.
This anticancer treatment is called photothermal therapy and generally involves packing tumors with nanoparticles that generate heat when exposed to near-infrared laser light. Human clinical trials have started on a gold-nanoparticle-based therapy for head and neck cancer, and now some research groups are exploring graphene-oxide-based therapies. Graphene oxide nanoparticles have some advantages over gold nanoparticles: They’re more efficient at converting near-infrared light into heat, and they cost less to make.
In photothermal methods, researchers typically inject nanoparticles into the bloodstream and then allow them to accumulate in tumors. But the particles also gather in organs such as the lungs and liver. Researchers want to limit this nonspecific accumulation with graphene, because the material’s toxicity is not fully understood, says Sei Kwang Hahn, a professor of materials science and engineering at Pohang University of Science & Technology, in South Korea.
Hahn and his colleagues thought that they could escort the graphene oxide nanoparticles directly to skin tumors by coupling them with hyaluronic acid, a sugar polymer that is found naturally in skin and is an ingredient in skin care products. The polymer can penetrate the skin’s top layer, and tumor cells are known to express a large number of hyaluronic acid receptors on their surfaces. So this coupling would allow the researchers to apply the graphene oxide particles to the skin, avoiding the need to inject them.
The researchers first tested how well their graphene oxide-hyaluronic acid packages penetrated skin. They dissolved the particles in water and then applied drops of the solution onto the skin of mice with and without implanted melanoma tumors. Confocal laser microscopy revealed that significantly more particles penetrated cancerous skin, which is more permeable than normal skin. This implies that the treatment would not affect healthy skin and underlying tissue, Hahn says.
Next, the team tested the solution’s ability to destroy tumors. The researchers applied the graphene oxide-hyaluronic acid solution onto the skin of mice implanted with two melanoma tumors, one on each side of their flanks. A few animals were treated only with graphene oxide nanoparticles for comparison. The researchers irradiated one side of the animals with near-infrared light for 10 minutes. They found that the tumors were completely destroyed only on the side treated with the graphene oxide-hyaluronic acid particles and near-infrared light. The researchers saw no recurrence of these treated tumors.
Fluorescence imaging of the extracted tumors showed that the conjugate particles penetrated 5 mm beneath the skin surface.
Treated skin turned black from the heat, but returned to normal a month after the treatment. Hahn says the team plans to investigate the conjugate particles’ safety and how the body clears the materials.
Delivering graphene oxide through the skin with the help of hyaluronic acid is a unique approach and a substantial advance, says Ravi N. Singh, a professor of cancer biology at the Wake Forest School of Medicine. The new technique might not be best for treating highly metastatic melanoma that might have spread to other parts of the body or superficial tumors that are easily removed by surgery, Singh says. But it could be an effective strategy against non-cancerous conditions and non-invasive cancers that cover large areas of the skin or are on the face, which are difficult to treat via injections, he says.



Join the conversation
Contact the reporter
Submit a Letter to the Editor for publication
Engage with us on Twitter