Advertisement
Grab your lab coat. Let's get started
Welcome!
Welcome!
Create an account below to get 6 C&EN articles per month, receive newsletters and more - all free.
It seems this is your first time logging in online. Please enter the following information to continue.
As an ACS member you automatically get access to this site. All we need is few more details to create your reading experience.
Not you? Sign in with a different account.
Not you? Sign in with a different account.
ERROR 1
ERROR 1
ERROR 2
ERROR 2
ERROR 2
ERROR 2
ERROR 2
Password and Confirm password must match.
If you have an ACS member number, please enter it here so we can link this account to your membership. (optional)
ERROR 2
ACS values your privacy. By submitting your information, you are gaining access to C&EN and subscribing to our weekly newsletter. We use the information you provide to make your reading experience better, and we will never sell your data to third party members.
Pharmaceuticals
Antibody-Antibiotic Duo Nabs Hidden Staph
Biotechnology: New biologic-drug conjugate targets Staphylococcus aureus stowing away inside host cells
by Judith Lavelle
November 4, 2015
| A version of this story appeared in
Volume 93, Issue 44

When Staphylococcus aureus, the most common cause of bacterial infections, sneaks into our bodies, it usually lives outside of our cells. But sometimes the microbes invade cells, possibly to hide out and survive antibiotic treatment—leading to persistent or relapsing infections.
Researchers at Genentech have now developed an antibody-antibiotic conjugate, or AAC, that targets S. aureus populations taking refuge in a host organism’s cells. Preclinical tests show that AACs are more effective than standard vancomycin treatments for clearing S. aureus infections in mice (Nature 2015, DOI: 10.1038/nature16057).
In the past few decades, researchers had reported evidence that successful human pathogens tend to escape into host cells, says Sanjeev Mariathasan, who led the Genentech team. “So the question was: ‘How do we kill these pathogens? Is that the reason we have these repeated infections?’ ”
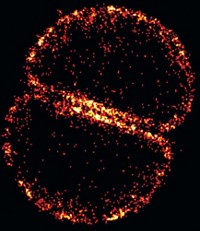
To start answering those questions, Genentech scientists first confirmed that these host cell reservoirs pose a significant problem by comparing mice infected with either free methicillin-resistant S. aureus (MRSA) or MRSA sequestered inside mouse immune cells. After four days without any treatment, many mice receiving the sequestered MRSA had higher bacterial burdens than those infected with free microbes. Also, standard MRSA treatments were unable to eliminate the sequestered bacteria.
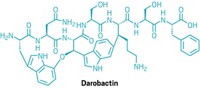
The scientists then created an anti-S. aureus antibody that binds to certain sugars on the surface of the bacteria. They attached a rifamycin-derived antibiotic called rifalogue to unpaired cysteines on the antibody with a linker molecule. Hundreds of these inactive AACs can attach to the surface of a bacterium before the coated bug invades a host’s immune cell. Once there, intracellular proteases cleave the linker molecule and release the AAC’s antibiotic cargo.
The AAC “turns the pathogen into a Trojan horse,” comments Kim Lewis, director of the Antimicrobial Discovery Center at Northeastern University, who was not involved in the study. “The antibiotic is released to kill both the incoming bacteria and those already present in mammalian cells,” he continues, adding that the strategy is a “genuinely novel approach to developing antimicrobials.”
S. aureus bacteria remain in a specific host cell for about two or three days before escaping into another. Mariathasan explains that the long half-life of the AACs allows them to latch onto bacteria throughout this process. “As long as these AACs are onboard in the patient,” he says, “they would then capture these bacteria and eventually put an end to the vicious cycle.”
In mice with systemic MRSA infections, the researchers found that one dose of AAC was able to clear the bacteria within 24 hours, beating out standard treatments of twice-daily vancomycin. Genentech currently has a patent on the technology, and Mariathasan says the group is “serious” about exploring the strategy in humans.
This article has been translated into Spanish by Divulgame.org and can be found here.



Join the conversation
Contact the reporter
Submit a Letter to the Editor for publication
Engage with us on Twitter