Advertisement
Grab your lab coat. Let's get started
Welcome!
Welcome!
Create an account below to get 6 C&EN articles per month, receive newsletters and more - all free.
It seems this is your first time logging in online. Please enter the following information to continue.
As an ACS member you automatically get access to this site. All we need is few more details to create your reading experience.
Not you? Sign in with a different account.
Not you? Sign in with a different account.
ERROR 1
ERROR 1
ERROR 2
ERROR 2
ERROR 2
ERROR 2
ERROR 2
Password and Confirm password must match.
If you have an ACS member number, please enter it here so we can link this account to your membership. (optional)
ERROR 2
ACS values your privacy. By submitting your information, you are gaining access to C&EN and subscribing to our weekly newsletter. We use the information you provide to make your reading experience better, and we will never sell your data to third party members.
Materials
Silk-based hydrogel could deliver sustained chemotherapy to tumors
An injectable hydrogel made with silk nanofibers releases breast cancer drug based on pH
by Deirdre Lockwood
July 12, 2016

An injectable hydrogel made with silk nanofibers could hold promise for delivering long-term chemotherapy directly to breast cancer tumors, a new study shows (ACS Appl. Mater. Interfaces 2016, DOI: 10.1021/acsami.6b04424). Researchers show that a silk hydrogel releases the breast cancer drug doxorubicin over two months in solutions that mimic the cellular environment, and keeps tumors at bay for five weeks in mice injected with the material.
Silk has long been used as a suture, but the low toxicity and unique biochemical properties of its fibrous protein, fibroin, have more recently led researchers to exploit it for other medical uses, including drug delivery. A few years ago, David L. Kaplan of Tufts University and his colleagues coaxed silk fibers to self-assemble into hydrogels that bind chemotherapeutic drugs and release them in a pH-dependent manner (Adv. Healthcare Mater. 2013, DOI: 10.1002/adfm.201201238). Though the system showed promise in mouse models of cancer, it had to be injected as a preformed gel. This meant that it could not surround a tumor, a more suitable therapeutic approach.
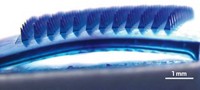
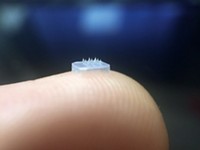
To develop such a system, Kaplan, Qiang Lu of Soochow University, and their collaborators built on recent work by others to create a semiliquid, silk-based hydrogel that can deliver doxorubicin. The gel is thixotropic, meaning it’s liquid when shaken and pushed through a syringe, so researchers can inject the gel around a tumor. After it’s injected, the gel no longer encounters such forces, so it solidifies around the tumor and releases the drug.
To make it, they first slowly concentrated a solution of silk fibroin derived from silkworms until nanoparticles formed. Then they diluted it with water and incubated the solution at 60 °C, generating nanofibers that cross-linked to form a hydrogel. Although the cross-linked network stabilizes the hydrogel, the nanofibers’ high charge density keeps them from aggregating, so the gel is semiliquid. Thus doxorubicin can be dissolved into it and allowed to bind to the silk nanofibers, and the system can be easily injected at the site of tumors.
Like many nanomedicine delivery methods, the system is designed to release the drugs at lower pH, as a way of targeting the more acidic environment surrounding cancer cells. In lab tests, the researchers found that the hydrogel rapidly released the drug over the first three weeks under all conditions, but unloaded the drug most completely over eight weeks at pH 4.5.
The team then tested the hydrogel delivery system in human breast cancer cell lines, where it inhibited cell growth for more than 10 days; in contrast, cells treated with doxorubicin alone began multiplying after the sixth day of the study. They also tested the system over five weeks in mice implanted with breast cancer tumors. For the first three weeks, all tumors treated with doxorubicin did not grow in weight or volume. Between week three and week five, mice given doxorubicin alone showed tumor growth while those who received the drug with the hydrogel delivery system did not.
Lakshmi Nair, a bioengineer at the University of Connecticut, says that getting sustained drug release from a hydrogel delivery system is a huge challenge: The gel is almost entirely water, so the drug tends to come out quickly through diffusion. She is impressed by the extended release the researchers achieved through the drug’s interaction with the silk network, together with the ability to inject it at the tumor site. “When you combine all these properties, she says, “it’s a very interesting strategy.” To bring this proof of concept toward the clinic, she says the researchers must see how effective it is compared with other delivery systems, such as nanoparticles or hydrogels using prodrugs.



Join the conversation
Contact the reporter
Submit a Letter to the Editor for publication
Engage with us on Twitter