Advertisement
Grab your lab coat. Let's get started
Welcome!
Welcome!
Create an account below to get 6 C&EN articles per month, receive newsletters and more - all free.
It seems this is your first time logging in online. Please enter the following information to continue.
As an ACS member you automatically get access to this site. All we need is few more details to create your reading experience.
Not you? Sign in with a different account.
Not you? Sign in with a different account.
ERROR 1
ERROR 1
ERROR 2
ERROR 2
ERROR 2
ERROR 2
ERROR 2
Password and Confirm password must match.
If you have an ACS member number, please enter it here so we can link this account to your membership. (optional)
ERROR 2
ACS values your privacy. By submitting your information, you are gaining access to C&EN and subscribing to our weekly newsletter. We use the information you provide to make your reading experience better, and we will never sell your data to third party members.
Biological Chemistry
Antibodies reverse synthetic opioid overdoses in mice
New approach counters the effects of fentanyl and carfentanil that overwhelm current overdose treatments like Narcan
by Tien Nguyen, special to C&EN
June 28, 2019
In a potential advance in treating opioid overdose, researchers have developed long-lasting monoclonal antibodies that selectively bind potent synthetic opioids and reverse their effects in mice. The researchers propose that the antibodies could one day be administered as a stand-alone treatment or as part of a more effective combination treatment against opioid overdoses (J. Amer. Chem. Soc.2019, DOI: 10.1021/jacs.9b04872).

Medical professionals have only one treatment option, a drug called naloxone, against acute opioid overdoses, which in 2017 killed more than 47,000 people in the US. The fast-acting treatment, sold as Narcan, races towards the brain where it blocks opioid receptors, denying the drugs access to them. But naloxone breaks down after about an hour, which allows a relapse into overdose unless the drug is readministered. Naloxone’s short lifetime also makes it less effective against powerful synthetic opioids like fentanyl and carfentanil, which are 100- and 10,000-fold stronger than morphine, respectively.

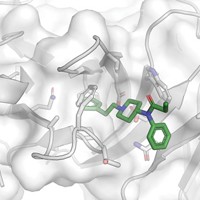
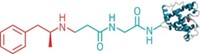
An antibody-based drug is one candidate for a more effective, longer lasting overdose treatment. To explore this possibility, a team at Scripps Research Institute led by Kim D. Janda first treated mice with a vaccine developed by their group in 2016 that stimulates the animals to produce a slew of different antibodies against fentanyl, some of which help protect the mice from overdoses (Angew. Chem. Int. Ed. 2016, DOI: 10.1002/anie.201511654). In the new work, the team recovered antibodies from the mice, purified them, and screened them for their ability to bind fentanyl. Although vaccines work by building up these antibodies for the next time opioids enter the body, in this case the researchers extracted the antibodies for direct use against an overdose. The team further evaluated six of these antibodies against nine fentanyl analogs commonly confiscated by law enforcement. One antibody, 6A4, demonstrated the best fentanyl binding affinity and had a six-day half-life in mice.
The team then compared 6A4 and naloxone’s ability to rescue mice from fentanyl and carfentanil’s effects. Mice received an opioid dosage expected to completely block pain followed half an hour later by an intravenous dose of either 6A4 or naloxone. To evaluate each treatment’s effectiveness, the team measured the animals’ response to pain using standard tests.
Both drugs reversed the opioid’s effects compared with mice that didn’t receive any treatment but naloxone’s effects kicked in earlier than 6A4, after about 1 h, which the researchers attribute to naloxone’s faster distribution through the body as a small molecule. Notably, 6A4 proved more effective than naloxone around 2 h after delivery, likely due to its longer half-life.
Naloxone works fast because it makes a beeline for opioid receptors in the brain, whereas antibodies like 6A4 can’t cross the barrier that separates the brain from the rest of the bloodstream. So Janda and colleagues propose that 6A4 sequesters synthetic opioids in the blood, creating an equilibrium imbalance that pulls more opioids from the brain into the bloodstream, where more antibodies await.
Combining 6A4 and naloxone could offer treatment that is both fast and long acting, Janda says. He adds that the antibody’s specificity for synthetic opioids avoids unwanted off-target binding to drugs like buprenorphine, which is used to help people reduce their opioid use.
Allegheny Health Network Research Institute’s Saadyah Averick, who has worked on extending naloxone’s lifetime using nanoparticles, says the work offers a “unique and orthogonal approach to sequester the potent synthetic opioids.” He says the antibodies’ specificity and longer circulation is interesting but wonders about the antibodies’ practicality as a treatment: biological therapies are much more expensive to make than small molecules, because they require special manufacturing facilities and storage, he says.
Although an antibody-based overdose drug would be more expensive than a drug like naloxone, the authors say, it would cost less than cancer immunotherapy, which is now routinely used to treat patients. Janda adds that the costs of making antibodies has significantly decreased over the past 10 years.
In the coming weeks, the team will test the antibodies’ ability to counter synthetic opioids’ effects in nonhuman primates, Janda says.
UPDATE
This story was updated on July 8, 2019, to clarify that the antibodies could one day be administered as a stand-alone treatment for opioid overdoses or as part of a combination treatment.



Join the conversation
Contact the reporter
Submit a Letter to the Editor for publication
Engage with us on Twitter