Advertisement
Grab your lab coat. Let's get started
Welcome!
Welcome!
Create an account below to get 6 C&EN articles per month, receive newsletters and more - all free.
It seems this is your first time logging in online. Please enter the following information to continue.
As an ACS member you automatically get access to this site. All we need is few more details to create your reading experience.
Not you? Sign in with a different account.
Not you? Sign in with a different account.
ERROR 1
ERROR 1
ERROR 2
ERROR 2
ERROR 2
ERROR 2
ERROR 2
Password and Confirm password must match.
If you have an ACS member number, please enter it here so we can link this account to your membership. (optional)
ERROR 2
ACS values your privacy. By submitting your information, you are gaining access to C&EN and subscribing to our weekly newsletter. We use the information you provide to make your reading experience better, and we will never sell your data to third party members.
Drug Development
Polymer could be a broader heparin blocker
A branching lysine polymer halts anticoagulant action of all types of heparin in plasma
by Louisa Dalton, special to C&EN
June 4, 2019

Doctors rely on the drug heparin, a blood thinner, to prevent blood clots during surgery and kidney dialysis. But they also rely on protamine, which binds heparin and blocks its action, to restore clotting when needed. Protamine has several disadvantages, though, so doctors would like an alternative. Chemists have now developed a promising substitute: a branched, all-lysine polymer that binds all three commonly used forms of heparin in plasma (ACS Med. Chem. Lett. 2019, DOI: 10.1021/acsmedchemlett.9b00090). The polymer needs to be tested for toxicity and effectiveness in animals to see if it could lead to a long-sought-after, universal heparin antidote.
Heparin, a carbohydrate polymer of varying chain lengths, binds to the antithrombin III enzyme, halting the cascade of reactions that cause blood to clot. But too much blood thinning can lead to uncontrolled bleeding, so in the operating room, surgeons always keep protamine, the only heparin antidote approved by the US Food and Drug Administration, on hand. Once surgery is over, they inject protamine to bind up and inactivate heparin, restoring blood clotting. The reversal agent is given to about 2 million heart bypass patients per year.
Protamine, however, is problematic, says Laurent Vial at University of Lyon. It is a mixture of small proteins isolated and purified from salmon sperm, and some patients have a severe allergic reaction or sudden low blood pressure in response to the drug. Worldwide supply is dependent on salmon availability. And although protamine binds unfractionated heparin, the type used for surgeries, it doesn’t work as well against two other types of heparin, which are often used to treat deep vein thrombosis, when blood clots form in the legs. If bleeding ensues after administering synthetic heparin (fondaparinux), which doesn’t bind protamine at all, physicians have no antidote. “There is strong incentive to find a new, safe substitute for protamine,” Vial says.
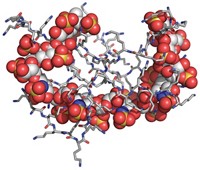
A handful of possible alternatives are now in preclinical and clinical stages. Vial, Gérald Monard of the University of Lorraine, Jean-Christophe Gris of the University Hospital of Nîmes, and their coworkers think they have an especially promising one: dendrigraft poly-L-lysine (DGL). DGL is a polymer made of lysine chains that looks like a hairy bush, with multiple branches sprouting off of one another. Each lysine holds one positive charge, so the DGL molecules they prepared varied from a one-branch version with a charge of +7 to their bushiest version at +727.
Unfractionated heparin carries the highest negative charge, about -90, of any biomolecule, so the scientists figured their DGLs would have a hard time staying away from it.
The researchers tested the idea by comparing DGLs of different sizes to protamine in their ability to halt heparin’s activity in plasma. The DGL with a charge of +41 worked best. It almost entirely reversed the blood-thinning action of unfractionated heparin and another form, low-molecular-weight heparin, more effectively than protamine in both cases. It also stopped about 60% of the action of synthetic heparin, which is not neutralized by protamine.
Based on molecular dynamics simulations, Vial says, the dendrigraft binds more efficiently than protamine because of its flexible branches. Protamine is like a stick, he says, made of one long amino acid chain. DGL’s branches get closer to heparin’s charges than protamine can.
David K. Smith, who studies heparin binding at the University of York, says that DGL “compares well to protamine in vitro. However, it will be essential to determine its toxicology and in vivo activity in the future.”
Jayachandran N. Kizhakkedathu of the University of British Columbia is also interested to see the dendrigraft activity in animal models. “Naked polycations are notorious for poor biocompatibility” and are often removed from action by the liver and spleen. Yet the work is encouraging because it neutralizes all types of heparins, he adds. An antidote with universal action and minimal toxicity that is economical and effective compared to protamine “would have significant clinical value.”




Join the conversation
Contact the reporter
Submit a Letter to the Editor for publication
Engage with us on Twitter