Advertisement
Grab your lab coat. Let's get started
Welcome!
Welcome!
Create an account below to get 6 C&EN articles per month, receive newsletters and more - all free.
It seems this is your first time logging in online. Please enter the following information to continue.
As an ACS member you automatically get access to this site. All we need is few more details to create your reading experience.
Not you? Sign in with a different account.
Not you? Sign in with a different account.
ERROR 1
ERROR 1
ERROR 2
ERROR 2
ERROR 2
ERROR 2
ERROR 2
Password and Confirm password must match.
If you have an ACS member number, please enter it here so we can link this account to your membership. (optional)
ERROR 2
ACS values your privacy. By submitting your information, you are gaining access to C&EN and subscribing to our weekly newsletter. We use the information you provide to make your reading experience better, and we will never sell your data to third party members.
Nanomedicines
Engineered ‘don’t eat me’ signal boosts nanoparticle uptake in cells
Liposomes carrying a chemical cue that curbs macrophages may improve nanoparticle drug delivery
by Alla Katsnelson, special to C&EN
November 26, 2019

Harnessing a signal used by the immune system to spare debris in the circulatory system from destruction may improve drug delivery using nanoparticles, according to a new early-stage study (ACS Nano 2019, DOI: 10.1021/acsnano.9b05679).
Medicine-carrying nanoparticles have to bypass many barriers in the body to ferry their cargo to where it is needed. One barrier is the so-called reticuloendothelial system—immune cells called macrophages that forage for dead cells, foreign material, and other debris in the liver, spleen, and circulatory system. Macrophages ingest and remove anything they find from the blood and thus “greatly limit the efficiency of nanomedicine,” says Chong Li, a drug delivery scientist at Southwest University in China.
To date, researchers have addressed this problem by coating nanoparticles in the widely used compound polyethylene glycol (PEG), which acts as a disguise for the particles, making macrophages avoid them. However, PEG also dampens the ability of target cells to bind to the particles.
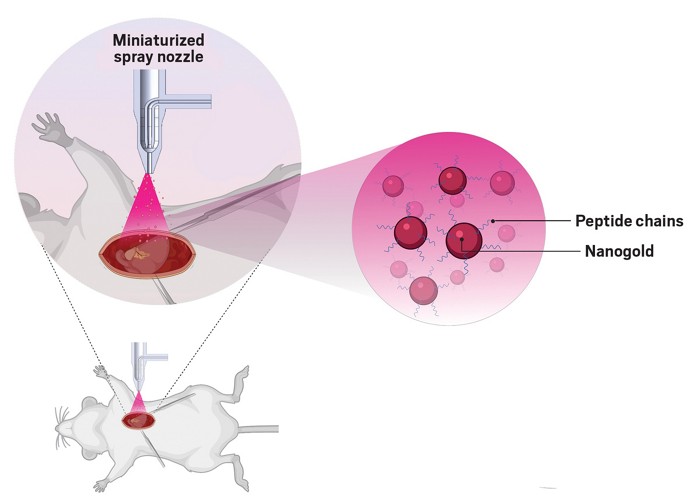
Li and his colleagues took a different approach. They made use of a glycoprotein, CD47, a protein produced by mammalian cells on their outer surfaces that binds to a receptor on macrophages. Macrophages that encounter CD47 recognize such cells as native to the organism: the protein is a “don’t eat me” signal. The researchers engineered liposomes to carry a short peptide sequence that mimics the active region of CD47.
The researchers speculated that if they inject these liposomes just before the drug-carrying nanoparticles, they could silence the macrophages and improve drug uptake. They first demonstrated that liposomes carrying the synthetic peptides bind to the macrophage receptor in cultured human cells. Next, they incubated mouse brain cells with both the liposomes and nanoparticles carrying a fluorescent label. They found that small amounts of the engineered liposomes do not interfere in nanoparticle uptake by the cells. Finally, the researchers showed that by injecting the liposomes into living mice that had a brain infection, they could increase the uptake of an antibiotic carried to the brain by nanoparticles to treat it.
The system has many potential benefits, Li says. For one thing, it can be used with any type of nanoparticle and any type of drug. For another, it’s very simple and doesn’t require complicated modifications to the drug delivery particles.
“It is an interesting piece of research—it has promise,” says Andre Nel, chief of nanomedicine at the University of California, Los Angeles. “But in my opinion, whether it is as simple as that will remain to be seen.”
Macrophages have a healing role at infection sites, and some studies suggest that macrophages near tumors boost a nanomedicine’s potency by engulfing nanoparticles and then releasing the drugs they carry. Silencing them widely with this strategy might therefore have a counterproductive effect, Nel says.
Li also notes that it is easy to use enough particles in a small organism like a mouse, but his team must still determine whether the approach will work in larger animals.


Join the conversation
Contact the reporter
Submit a Letter to the Editor for publication
Engage with us on Twitter