Advertisement
Grab your lab coat. Let's get started
Welcome!
Welcome!
Create an account below to get 6 C&EN articles per month, receive newsletters and more - all free.
It seems this is your first time logging in online. Please enter the following information to continue.
As an ACS member you automatically get access to this site. All we need is few more details to create your reading experience.
Not you? Sign in with a different account.
Not you? Sign in with a different account.
ERROR 1
ERROR 1
ERROR 2
ERROR 2
ERROR 2
ERROR 2
ERROR 2
Password and Confirm password must match.
If you have an ACS member number, please enter it here so we can link this account to your membership. (optional)
ERROR 2
ACS values your privacy. By submitting your information, you are gaining access to C&EN and subscribing to our weekly newsletter. We use the information you provide to make your reading experience better, and we will never sell your data to third party members.
Spectroscopy
Raman techniques might one day allow blood banks to monitor the quality of their supplies
Spectroscopy methods could provide clues to health of stored red blood cells, studies show
by Celia Henry Arnaud
April 12, 2019
| A version of this story appeared in
Volume 97, Issue 15

Every year in the US, about 6.8 million people donate blood. After a person donates blood, the clock starts ticking for its ingredients—the plasma, platelets, and red blood cells—that might be transfused into a patient. Just like any biological matter, they have a shelf life. They degrade. In the case of red blood cells, for instance, hospitals and blood banks have up to 42 days to use them as long as they’ve been refrigerated properly.
That shelf life, though, is set by the blood bag manufacturers, not by measuring the quality of blood over time, but by measuring the time that transfused blood cells last inside a healthy person’s body. No one really knows the quality of blood stored for the full shelf life. Biochemically speaking, researchers don’t have a solid idea of what the indicators are of “good” blood versus “bad” blood.
What blood experts do know is that, as blood ages, it acquires what is known as “the storage lesion,” the accumulation of changes to the red blood cells during storage, many of which are caused by oxidative damage. Currently there’s no way to test for this damage in blood that’s been stored inside a bag without opening the bag, compromising its sterility, and rendering the blood unusable. Even if there were testing methods, people still don’t know whether such changes in the blood correlate with poor patient outcomes.
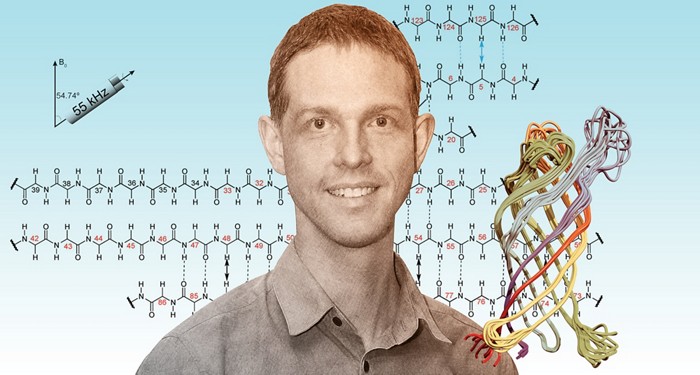
But an option could be available soon. Two independent teams—one led by Robin F. B. Turner and Michael W. Blades of the University of British Columbia (UBC) and the other led by Richard A. Dluhy of the University of Alabama at Birmingham (UAB)—are working to develop Raman spectroscopy as a method that can monitor blood inside storage bags without ever opening them.
Turner and Blades became interested in analyzing stored blood after they met Dana V. Devine, a pathology professor at UBC and the chief scientist at Canadian Blood Services, Canada’s blood banking agency. About a decade ago, Devine says, transfusion medicine specialists started worrying about the quality of blood products in the late stages of their shelf lives. They thought blood recipients might have worse outcomes when they were given blood products that had been stored for 5 or 6 weeks instead of a couple of weeks. Prospective trials, such as the Age of Blood Evaluation trial, have allayed some of those concerns, showing that the age of transfused blood has little or no effect on patient outcomes (N. Engl. J. Med. 2015, DOI: 10.1056/nejmoa1500704).
“That’s good news for organizations like mine,” Devine says. “But it also got us focused on what’s actually in that bag of red blood cells.”
Sure, on average, fresh blood and weeks-old blood are both OK for patients under most circumstances, but the blood in some bags could still go bad earlier than the blood in others. Devine likens it to the expiration date on a carton of yogurt. Some yogurt remains good past the printed expiration date, whereas other yogurt goes bad before that date. A color change or smell can indicate to consumers if they’ve gotten a bad yogurt, but for donated blood, it’s not easy to tell, especially because the bag needs to stay closed.
Through their connection at UBC’s Centre for Blood Research, Devine teamed up with Turner and Blades to see whether the pair’s Raman methods could be useful.
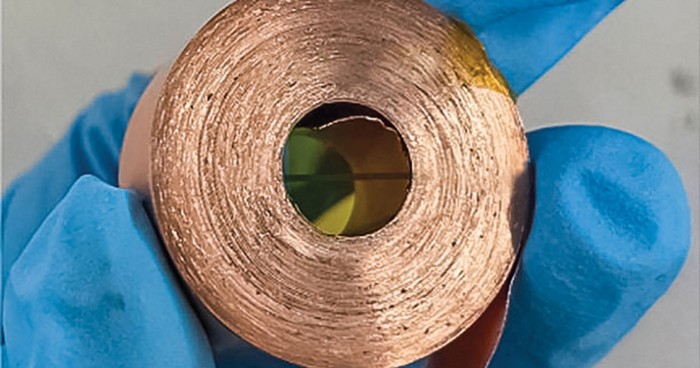
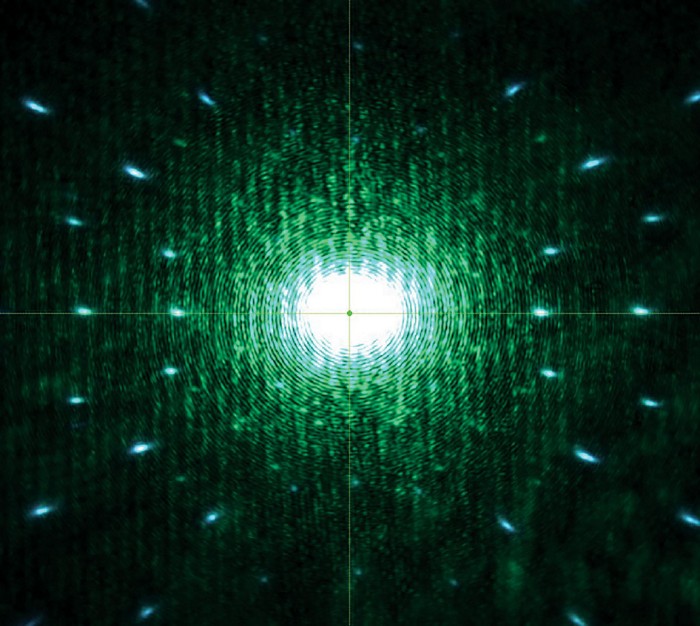
Their method of choice is called spatially offset Raman spectroscopy (SORS), which can collect Raman spectra from beneath translucent surfaces, such as the polymer that makes up blood storage bags. In SORS, an excitation beam is directed into a sample, and Raman scattered photons are collected from two locations—one at the same spot as the excitation beam and another at a location offset by a few millimeters. This strategy allows the collection of Raman spectra from molecules below the surface.
Before the UBC team could analyze blood through a bag, it first needed to directly analyze blood removed from bags. “It was the best way for us to begin our learning curve about how the blood changes,” Turner says.
“Our red cells have a lot of hemoglobin,” Turner says. Spectral bands from hemoglobin can mask other spectral markers the researchers would like to identify that correlate with the chemistry and physiology of blood cells. “We’re trying to figure out ways to see between the hemoglobin bands more clearly and get additional information from the suspended cells.”
One promising marker of blood cells’ health is lactate. Blood cells are stored in a solution of glucose and other additives. When cells metabolize glucose under low-oxygen conditions, like those in a storage bag, they produce lactate as a waste product. In blood storage bags, that lactate collects in the supernatant liquid above the cells that have precipitated to the bottom. Preliminary work suggests that lactate levels change over the course of storage and that some stored blood units accumulate lactate more readily than others. Thus, lactate might be a biomarker for blood quality (Analyst 2016, DOI: 10.1039/c6an00373g).
Despite the challenges of hemoglobin, Turner and Blades are also looking at it as a possible marker of storage-induced changes in blood. They’re primarily focusing on the ratio of deoxygenated to oxygenated hemoglobin in samples. Raman spectra reveal changes in hemoglobin oxygenation that appear to correlate with morphological changes in the blood cells (Analyst 2017, DOI: 10.1039/c7an00349h).

As they’ve continued studying stored blood, Turner and Blades have demonstrated that they can indeed analyze blood directly in the storage bags by monitoring the ratio of deoxyhemoglobin to oxyhemoglobin (Analyst 2018, DOI: 10.1039/c8an01509k).
But they’re not entirely satisfied with SORS yet. One problem that Turner and Blades have found is that commercial SORS instruments are optimized to analyze more highly concentrated samples than the components in blood storage bags. They would also like to be able to adjust the offset. “We would like to be able to turn some knobs and optimize the instrument. Because it’s a commercial instrument, it’s not easy to do that,” Turner says. “We’re doing the best we can with what we’ve got. We’ve learned a few tricks to improve things, but it’s still not optimal.”
Dluhy and his team at UAB, including Rakesh P. Patel in the School of Medicine, have also tried SORS for analyzing stored blood but found that it wasn’t yielding enough signal for the molecular components they wanted to study. The group has instead turned to a different Raman method called resonance Raman spectroscopy, which uses a red excitation beam at 632 nm excitation. This wavelength coincides with an electronic transition of hemoglobin and thus provides a resonant enhancement in the signal that comes from blood samples. To adapt the method for storage bags, Dluhy and his team defocus the excitation laser beam and change detector settings to collect Raman scattered photons from deeper in the sample. They call their adapted technique diffuse resonance Raman spectroscopy.
The UAB researchers are using diffuse resonance Raman to measure oxygenated hemoglobin and another form of hemoglobin called methemoglobin to see whether they can detect the rupture, or hemolysis, of red blood cells through a storage bag. In methemoglobin, the iron in the heme group is in the ferric (+3) state rather than the ferrous (+2) state of normal, oxygenated hemoglobin. Methemoglobin is attractive as a potential marker because it’s usually a minor form of hemoglobin, so changes in its abundance could make it a selective indicator of storage-related changes.
In a preliminary study, the team repeatedly sampled blood from the same six donors at 7, 21, and 35 days of storage and analyzed it with conventional Raman spectroscopy (Lab Med. 2018, DOI: 10.1093/labmed/lmy018). The researchers found that levels of both oxyhemoglobin and methemoglobin increased during the storage period.
“We’ve been able to show that the predominance of methemoglobin is an indicator of hemolysis and toxicity in red blood cells,” Dluhy says. “We have to do a lot more studies correlating the spectroscopy with the biochemistry of what’s going on in the bag. Hopefully, we’ll be able to do something like that in the near future.”
In another study, the UAB researchers used diffuse resonance Raman to analyze blood not in the storage bags themselves but in segments of polymer tubing connected to and made of the same material as the blood bags. They were able to spectrally distinguish blood that had been stored 6–8 days from blood that had been stored 35–40 days (Analyst 2018, DOI: 10.1039/c8an01135d).
After the technology that both the UBC and UAB teams are working on gets to a level where it can be used routinely, Devine imagines blood banks will regularly monitor the status of their supplies. Blood cells that look like they’re metabolizing quickly could be moved to the front of the inventory to be used before they go bad.
“There’s a clear need for label-free, noninvasive, and sensitive techniques that can assess the quality of red blood cells during storage,” Dluhy says. He thinks the early results indicate that Raman could meet that need. But those early results need to be reproduced, he says. “There needs to be a lot more correlative work to convince not just spectroscopists but biochemists, pathologists, and the medical community that this is something they can reliably use and trust.”


Join the conversation
Contact the reporter
Submit a Letter to the Editor for publication
Engage with us on Twitter